 NIK LEBOWSKI/ISTOCK/GETTY IMAGES PLUS
NIK LEBOWSKI/ISTOCK/GETTY IMAGES PLUS
Aerosol Control Using Dental Extractor Technology
Equipping operatories with portable extraoral aerosol extractors can improve the safety of care by helping contain dental bioaerosols.
This course was published in the November 2021 issue and expires November 2024. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATIONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain dental aerosols and spatter, and concerns over aerosol-generating procedures in light of the COVID-19 pandemic.
- Describe mitigation strategies that can help control spatter and aerosols in dental settings.
- Discuss key factors in the purchase decision when introducing a dental aerosol extractor to the clinic.
As policymakers, healthcare officials, clinicians, and the general population wrestle with the impact of highly virulent strains of COVID-19, feelings of uncertainty, fear, and confusion remain in many homes and workspaces. In light of the increased transmission rates and disease severity associated with these strains, independent sources — such as the Coronavirus Resource Center at John Hopkins University1 — continue to track daily morbidity and mortality on a national and global scale. The impact of COVID-19 is particularly problematic in clinical oral health settings due to spatter and aerosols produced by power-driven dental instruments. Although it has yet to be proven whether dental aerosols from SARS-CoV-2-infected individuals contain viral loads sufficient to cause cross-transmission, until such time this is scientifically and definitively proven or refuted, aerosols should be considered potentially infectious and controlled as much as possible.
In light of this, the Occupational Safety and Health Administration’s (OSHA) occupational risk pyramid for exposure to COVID-19 places dentists and dental hygienists in the “very high risk” category.2 A variety of equipment and instruments used by dental professionals can generate aerosols and spatter. Consequently, the pandemic has sparked increased interest in technologies designed to control these emissions, including portable extraoral dental aerosol extractors.
While the definition of particle sizes regarding spatter and aerosols is controversial, this paper will use the definitions of spatter and droplets provided by Gallagher et al3 and Atkinson et al.4 When the particle size is larger than 50 micrometers (μm), it is defined as spatter.3 However, when the particle size is bigger than 5 μm, it is called a droplet.3 Additionally, if the particle size is less than 5 μm, it is called a droplet nuclei.4
Researchers have utilized particles in the range of 10 to 20 μm to evaluate the spread of dental aerosols and potential contamination of patients and providers during aerosol-generating procedures;5 these evaluations have also examined the suctioning effectiveness of extraoral dental aerosol extractors.6 It is possible that dental aerosols might contain opportunistic pathogens that can be detrimental to health, especially for immunocompromised patients. Moreover, particle size matters when assessing infection risk; the smaller the aerosol particles (0.5 to 10 μm), the greater the risk of a pathogenic microorganism penetrating and lodging into the smaller passages of the lungs.7

Bioaerosol Removal Via Portable Devices
Studies show that use of ultrasonic scaling devices, dental handpieces, and three-in-one air/water syringes increases bioaerosol levels.7 Most of these bioaerosols come from a variety of sources, such as blood, saliva, plaque, calculus, and poorly disinfected dental unit waterlines. Oral health professionals may be at greatest risk when treating patients with heavy supra- and/or subgingival calculus since reports indicate the ultrasonic scaler is the greatest contributor to aerosols and spatter.8,9 In today’s practice environment, a new wave of improved extraoral dental aerosol extractors is being utilized to combat the spread of aerosols. Interest in aerosol extractors has likely increased due to the COVID-19 pandemic, and researchers continue to assess the efficacy of these devices as adjunctive aids in infection prevention.
The U.S. Centers for Disease Control and Prevention (CDC), OSHA and the American Dental Association have recommended optimizing engineering controls if aerosol-generating procedures cannot be postponed as part of efforts to minimize spatter and aerosolization during dental treatment.10–12 While portable extraoral aerosol extractor systems are not specifically identified, their use may be an additional engineering control to consider to mitigate spray and spatter into the dental environment during aerosol-generating procedures. Understandably, interest in studying their effectiveness in removing bioaerosols increases as more virulent strains of SARS-CoV-2 emerge, warranting better understanding of aerosol extractors’ role in reducing exposure among providers and patients to viruses and other particulate infectious materials that may contaminate the dental environment.
Filtration Mechanisms
The technology behind dental aerosol extractors varies depending on the manufacturer, but most utilize filtration stages that purify the air before it is released back into the room. At their core, most extractors use various types of high efficiency particulate air (HEPA) filters. Filters must meet specific criteria in order to be labeled as HEPA units. A HEPA filter must remove at least 99.95% (European standard) to 99.97% (U.S. standard) or more of all particles that are 0.3 microns (μm) in diameter.13 Extrapolating from a 2016 NASA report on HEPA filtration efficiency,14 the biggest clinical impact of these filters is their potential for use against SARS-CoV-2. Although not written in the context of COVID-19, the paper states, “HEPA filters are nearly 100% efficient at capturing the spectrum of particles down to the very smallest airborne particulates.”14 Additionally, current research suggests that adding HEPA filtration in high-risk environments can enhance indoor air cleaning, thus reducing the spread of pathogenic organisms.15 The CDC notes that 0.3 µm approximates the most penetrating particle size (MPPS) through a HEPA filter, but adds, “HEPA filters are even more efficient at capturing particles larger and smaller than the MPPS. Thus, HEPA filters are no less than 99.97% efficient at capturing human-generated viral particles associated with SARS-CoV-2.”15

Key Features
Most extractors utilize multiple filtration stages; for example, a dental aerosol extractor may offer as many as five stages of air filtration. Some units have suction-rate speed settings that can be adjusted depending on the planned procedure and expected aerosol escape from the oral cavity. Suction rate is measured in cubic feet per minute (CFM), and can range from 50 to 350 CFM. Purchase considerations for portable aerosol extractors include suction efficiency and cost, which varies from $1500 to $3000 per unit. Features also vary by model, and each company may offer options that can help tailor the equipment to meet usage requirements and operator preference.
Additional factors to consider include the size of the unit (i.e., projected fit within the operatory), portability, efficacy of air filtering, presence of articulated bends (Figure 1) in the unit’s arms (which may impact airflow), noise level, and having well-sealed, encased HEPA filters that prevent contaminated air from leaking outside the unit. Space considerations in various operatories may dictate the use of smaller extractors (Figure 2), and clinicians should also consider the ease of rotating and repositioning the unit’s arms for optimal access during treatment.
Noise levels while utilizing external oral suction can range from 50 to 75 decibels (dB).16 This can directly impact communication between dental teams and patients. For comparison purposes, Qsaibati and Ibrahim17 determined the highest noise level measured during dental clinic operation was from a micromotor handpiece cutting on acrylic, which produced 92.2 dB, while the ultrasonic scaler generates 51.7 dB. For perspective, OSHA requires ear protection at 85 dB.18 Consideration for ear protection to prevent hearing loss among patients and providers is warranted given the noise generated from extraoral dental aerosol extractors when used in combination with handpieces and ultrasonic/power scaling devices.
Combining Bioaerosol Reduction Strategies
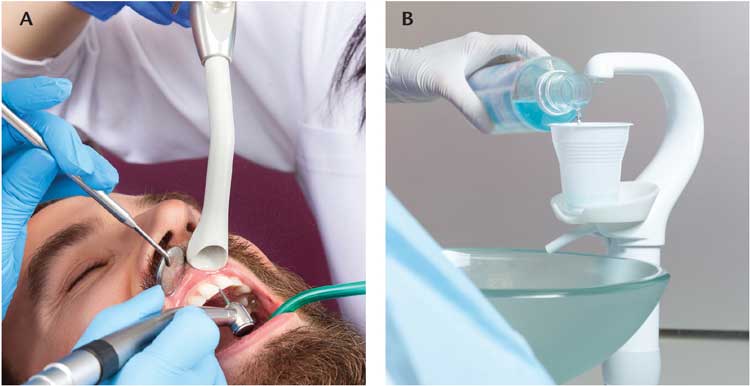
In its guidelines for optimizing the use of engineering controls, the CDC recommends that oral health professionals consider mitigation strategies — such as using four-handed dentistry, high-evacuation suction and dental dams — to minimize droplet spatter and aerosols.10 Current research findings indicate that extraoral vacuums are effective in reducing spatter6 and aerosols.5 Regardless, the use of an extraoral dental aerosol extractor alone is insufficient in reducing bioaerosols and spatter within the dental environment. Instead, this technology is recommended as an adjunct in conjunction with other techniques and procedures that can help eliminate the spread of bioaerosols. Studies show that in combination or alone, utilizing dental dams, four-handed dentistry,19,20 high-volume wide-bore aspiration (typically referred to as high-volume evacuators), and preprocedural antiseptic mouthrinses can effectively reduce the risk of infection from airborne contaminates.21 Specifically, aspiration can reduce airborne bacterial contamination by more than 90%, while using an appropriate antiseptic mouthrinse has also been shown to significantly reduce the bacterial count in the air (Figures 3A and 3B).21
Unit Infection Control
Disinfecting an extraoral dental aerosol extractor between patients is a necessary component of an effective infection prevention protocol. Each manufacturer has varying methods for disinfecting the unit. For example, the extraoral vacuum unit can typically be disinfected after each patient use by positioning the hood facing up and spraying disinfecting solution into the suction mouthpiece hood for 10 seconds and then running the vacuum for three minutes at a setting of 1–2. Next, the suction mouthpiece hood is removed from the arm and placed in a sterilization pouch for autoclaving. The external controls, arm, handles, and exterior surfaces of the unit are wiped with a disinfecting cloth to clean, and then a second time with a new disinfecting cloth to disinfect and prepare the unit for subsequent use. Placing dental barrier film on the external control settings and handles (if equipped) helps prevent cross-contamination when the unit is turned on/off or during suction adjustment, and also if the unit needs to be moved during patient treatment.
Conclusion
Both before and throughout the COVID-19 pandemic, oral health professionals have conscientiously worked to prevent cross-contamination and maintain meticulous aseptic protocols to keep patients and providers safe. As more research is conducted on viral transmission through aerosols — as well as preventive measures to reduce aerosolized infectious materials — it is likely that additional technologies will be developed to safeguard the air in dental environments.
Such innovations will augment existing standards for infection prevention in oral healthcare, including preprocedural regimens, precautions during treatment, and postprocedural protocols. That said, the COVID-19 pandemic has sparked renewed interest in controlling bioaerosols and spatter. Toward this goal, dental aerosol extractors are an adjunctive technology that can be considered in conjunction with other aseptic techniques to combat the spread of SARS-CoV-2 or other transmissible pathogens emanating from the oral cavity and/or respiratory tract.
It is likely that heightened urgency in developing effective aerosol extractors will continue as part of efforts to mitigate risks posed by airborne particles generated during dental procedures. This is especially relevant as dental teams continue to address the demand for care, and work through a backlog of patients who delayed treatment as a result of COVID-19.
As the profession continues to learn from the pandemic, clinicians can consider implementing new technologies to support safe treatment — and work to be better prepared to handle future disease outbreaks.
References
- Johns Hopkins University. Coronavirus Resource Center. Available at: https://coronavirus.jhu.edu/map.html. Accessed September 29, 2021.
- Mupparapu M. Editorial: Aerosol reduction urgency in post-COVID-19 dental practice. Quintessence Int. 2020;51:525–526.
- Gallagher JE, Sukriti KC, Johnson IG, et al. A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open. 2020;6:25.
- Atkinson J, Chartier Y, Pessoa-Silva CL, et al. Natural ventilation for infection control in health-care settings — Annex C, respiratory droplets. Available at: https://www.ncbi.nlm.nih.gov/books/NBK143281/. Accessed September 29, 2021.
- Yang M, Chaghtai A, Melendez M, et al. Mitigating saliva aerosol contamination in a dental school clinic. BMC Oral Health. 2021;21:52.
- Chavis SE, Hines SE, Dyalram D, Wilken NC, Dalby RN. Can extraoral suction units minimize droplet spatter during a simulated dental procedure? J Am Dent Assoc. 2021;152:157–165.
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135:429–437.
- Veena HR, Mahantesha S, Joseph PA, Patil SR, Patil SH. Dissemination of aerosol and splatter during ultrasonic scaling: A pilot study. J Infect Public Health. 2015;8:260–265.
- Harrel SK. Ultrasonic aerosols in the age of COVID-19. Decisions in Dentistry. 2020;6(7):21–24.
- U.S. Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Accessed September 29, 2021.
- Occupational Safety and Health Administration. Dentistry Workers and Employers. Available at: https://www.osha.gov/coronavirus/control-prevention/dentistry. Accessed September 29, 2021.
- American Dental Association. As Dental Practices Resume Operations, ADA Offers Continued Guidance. Available at: https://www.ada.org/en/press-room/news-releases/2020-archives/may/as-dental-practices-resume-operations-ada-offers-continued-guidance. Accessed September 29, 2021.
- Robertson P. What Are HEPA Filters and How Do They Work? Available at: https://smartairfilters.com/en/blog/what-is-hepa-filter-how-hepa-filter-work/. Accessed September 29, 2021.
- Perry JL, Agui JH, Vijayakumar R. Submicron and Nanoparticulate Matter Removal by HEPA-Rated Media Filters and Packed Beds of Granular Materials. Available at: https://ntrs.nasa.gov/api/citations/ 20170005166/downloads/20170005166.pdf. Accessed September 29, 2021.
- U.S. Centers for Disease Control and Prevention. Ventilation in Buildings. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html. Accessed September 29, 2021.
- American Association of Oral and Maxillofacial Surgeons. Intraoral vs. Extraoral Suction Devices. Available at: https://www.aaoms.org/news/intraoral-vs-extraoral-suction-devices. Accessed September 29, 2021.
- Qsaibati MhdL, Ibrahim O. Noise levels of dental equipment used in dental college of Damascus University. Dent Res J (Isfahan). 2014;11:624–630.
- Occupational Safety and Health Administration. Occupational Noise Exposure. Available at: https://www.osha.gov/noise. Accessed September 29, 2021.
- Senpuku H, Fukumoto M, Uchiyama T, Taguchi C, Suzuki I, Arikawa K. Effects of extraoral suction on droplets and aerosols for infection control practices. Dent J. 2021;9:80.
- Graetz C, Düffert P, Heidenreich R, Seidel M, Dörfer CE. The efficacy of an extraoral scavenging device on reducing aerosol particles ≤ 5 µm during dental aerosol-generating procedures: an exploratory pilot study in a university setting. BDJ Open. 2021;7:1–7.
- Hallier C, Williams DW, Potts AJ, Lewis MA. A pilot study of bioaerosol reduction using an air cleaning system during dental procedures. Br Dent J. 2010;209:E14.
From Decisions in Dentistry. November 2021;7(11)40-43.




