
Ensuring Effective Periodontal Maintenance
Clinicians must regularly reassess periodontal maintenance to ensure it meets or exceeds standards. Learn why thorough evaluation and adaptation of treatment approaches are essential for optimal oral health.
Clinicians should strive to deliver periodontal maintenance that meets or exceeds the norm. In that effort, repeated reassessment is necessary to determine if different approaches are warranted. Assessment of nonsurgical therapy is complicated by three variables. First, removing all subgingival biofilm and calculus is demanding — and may be impossible. Second, detecting subgingival calculus is challenging. Third, the quality of self-care is inconsistent. Absent good self-care, it is difficult to determine whether persistent signs of inflammation are caused by supra- or subgingival etiologies.
Sherman et al1 looked at the detection of subgingival calculus via tactile perception. They reported a high false negative response (77.4%) when comparing clinical reports of calculus-free root surfaces versus low-magnification microscopic evaluation of those same surfaces. Tactile perceptions of the subgingival environment lack sensitivity, specificity and reproducibility. Put simply, if root calculus cannot be seen, it cannot be reliably detected. And even if detected, the inability to see the tooth surface offers no assurance the calculus has been removed. This often results in residual calculus and over-instrumentation (excessive removal of cementum or dentin — or both).
The interval between completion of nonsurgical periodontal therapy (ie, scaling and root planing [SRP]) and the first reevaluation appointment should be long enough to allow near-complete healing of treated sites. The connective tissues of an inflamed gingival lamina propria may require as many as 12 weeks of healing following SRP. Reevaluation is not an endpoint, but a waypoint. Additionally, reevaluation of any periodontal treatment, including SRP, requires a reassessment of the same clinical parameters used to diagnose disease and construct the original treatment plan.2
Two important aspects of reassessment can be viewed in the context of research that revealed bleeding on probing is not a completely reliable prognostic indicator for subsequent attachment loss, and sites consistently free of bleeding on probing (the desired results of adequate SRP, combined with good self-care) will not incur subsequent attachment loss.3 This research provides an important clinical goal; however, the investigation was of limited duration, which further suggests the presence of persistent bleeding on probing bodes poorly for a site.
Along the same lines, special attention must be focused on furcation involvements, particularly those with bleeding on probing. This is because such sites may experience rapid attachment loss. Long-term data reveal that furcation involvement approximately doubles the risk of tooth loss for molars over 10 to 15 years. In spite of this observation, most molars with a furcation involvement will respond favorably to periodontal therapy if adequately instrumented and in the presence of good self-care that result in consistent elimination of bleeding on probing.
Next Steps
Results of reassessment determine the next steps in treatment. This is likely to be periodontal maintenance or a second SRP at nonresponding, still-diseased sites. A second SRP is often more successful if performed using advanced instrumentation designed to improve operator visibility. The second SRP should be followed by another reevaluation appointment. If diseased sites persist at this appointment (generally assessed by the presence of bleeding on probing), the next step may be surgical intervention.

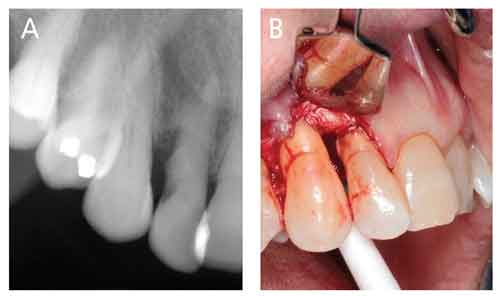
Surgical treatment typically seeks improved access for removal of subgingival calculus and biofilm. Figure 1 depicts the limits to blind SRP, despite radiographs that show subgingival calculus. Here, the dental hygienist did a good job of blind SRP, but the nearby periodontium continued to display signs of inflammation upon reevaluation. Access surgery was performed. Note the discoloration at cementoenamel junction sites, suggesting retained calculus, as well as sheets of thin, brownish calculus on root surfaces apical to those debrided via blind SRP. Figures 2A and 2B depict a similar situation in a different patient.
Some surgeries may also employ regenerative technologies or tissue sculpting aimed at providing better support or tissue anatomy that is more easily maintained. Other surgical procedures may improve appearance and mitigate chronic pain. In recent years, minimally invasive surgeries have facilitated improved SRP and regenerative opportunities at some sites, but they necessitate use of advanced instrumentation that improves visualization and instrumentation.
Like other chronic diseases, the ongoing nature of periodontitis requires meticulous reevaluations and modulation of subsequent care, including maintenance. The initial interval between maintenance appointments should be based on a patient’s risk for disease recurrence. Factors such as residual probing depths, persistent bleeding on probing, erratic or inadequate self-care, and failure to attend periodontal maintenance visits point to increased risk.4
Unfortunately, many practices still adhere to a soft-tissue management protocol consisting of SRP, a 4- to 6-week reevaluation, and near-automatic assignment to a periodontal maintenance program with 6-month intervals. Although this may succeed for a few patients and insurance companies, it will not work for most. Dockter et al5 reported that treatment of periodontitis in general dental practices varied little regardless of disease severity or risk of subsequent disease. They also reported the average number of periodontal maintenance appointments was fewer than what research suggests is appropriate for patients with moderate to advanced periodontitis. In fact, periodontal diseases are often not managed properly or in a timely manner.5,6 If clinical procedures, such as SRP, do not produce desired results, other therapies should be considered, as should referral to a specialist.
The effectiveness of SRP and patient-centered maintenance is supported by a 2015 American Dental Association-commissioned systematic review and clinical practice guidelines that addressed the nonsurgical treatment of periodontitis with or without adjunctive therapies.7,8 On average, SRP is a remarkably effective treatment if executed with precision by skilled clinicians.
Conclusions
Based on published evidence, the following conclusions are reasonable:
- Subgingival calculus and root surface irregularities are replete with biofilm composed of metabolically active bacteria.
- Removing subgingival bacterial and calculus helps create biologically compatible root surfaces. Thorough and judicious root planing can eliminate such deposits. Endotoxin adsorbs to tooth surfaces but is easily removed once deposits are eliminated. Numerous clinical studies have documented the beneficial effects of complete removal of subgingival calculus on the resolution of inflammation.9
- Periodontal destruction appears related to the presence of calculus.10-14
- Effective SRP is difficult, especially in sites with deeper probing depths. It can often be performed well only by highly skilled clinicians who may need advanced instrumentation to ensure appropriate visualization of subgingival tooth surfaces.15-17 Additionally, effective SRP demands thorough calculus removal. Complete removal of subgingival cementum should not be a goal of periodontal therapy but is often inevitable.18
- Inflammation associated with periodontitis adversely affects not only the oral environment, but also systemic health. This observation reinforces the importance of effective SRP, high-quality self-care, appropriate reevaluations, and further treatment if indicated. The need for periodontal maintenance remains as long as patients have teeth (or implants). Initial maintenance intervals should trend toward too often, rather than too seldom — with an eye toward increasing maintenance intervals if clinical needs dictate.
- Goals of SRP include complete removal of calculus and biofilm, smoothing root surfaces, eliminating bleeding on probing (which necessitates effective self-care), reducing probing depths, increasing clinical attachment levels, and eliminating inflammation, thereby reducing the systemic inflammatory burden.
- An astute clinician will treat periodontitis using appropriate instrumentation, monitor results of treatment via periodic reevaluations, and perform appropriate and timely treatments and retreatments of recurrent disease as needed.19
- Finally, SRP is one of numerous approaches available to arrest periodontitis and restore health. If a single session or multiple sessions of SRP do not achieve waypoints indicative of health and stability, other therapies must be provided — including referral to a specialist if indicated.
References
- Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planing. I. Clinical detection of residual calculus. J Periodontol. 1990;61:3–8.
- Claffey N. Decision making in periodontal therapy. The re-evaluation. J Clin Periodontol. 1991;18:384–389.
- Lang NP, Adler R, Joss A, Nyman S. Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol. 1990;17:714–721.
- Ramseier CA, Nydegger M, Walter C, et al. Time between recall visits and residual probing depths predict long‐term stability in patients enrolled in supportive periodontal therapy. J Clin Periodontol. 2019;46:218–230.
- Dockter KM, Williams KB, Bray KS, Cobb CM. Relationship between pre-referral periodontal care and periodontal status at time of referral. J Periodontol. 2006;77:1708–1716.
- Cobb CM, El-Annan E, Carrara A, et al. Periodontal referral patterns, 1980 vs 2000: a preliminary study. J Periodontol. 2003;74:1470–1474.
- 7. Smiley CJ, Tracy SL, Abt E, et al. Systematic review and meta-analysis on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:508–524.
- Smiley CJ, Tracy SL, Abt E, et al. Evidence-based clinical practice guideline on the nonsurgical treatment of chronic periodontitis by means of scaling and root planing with or without adjuncts. J Am Dent Assoc. 2015;146:525–535.
- Cobb CM. Non-surgical pocket therapy: mechanical. Ann Periodontol. 1996;1:443–490.
- Adriaens PA, Adriaens LM. Effects of nonsurgical periodontal therapy on hard and soft tissues. Periodontol 2000. 2004;36:121–145.
- Quirynen M, De Soete M, Dierickx K, van Steenberghe D. The intra-oral translocation of periodontopathogens jeopardizes the outcome of periodontal therapy. A review of the literature. J Clin Periodontol. 2001;28:499–507.
- Wilson TG, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies — a pilot study. J Periodontol. 2008;79:2036–2041.
- Wilson TG, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planing using the dental endoscope: human biopsies — a pilot study. J Periodontol. 2008;79:2036–2041.
- Mandel ID. Calculus update: prevalence, pathogenicity and prevention. J Am Dent Assoc. 1995;126:573–580.
- Kuang Y, Hu B, Chen J, Feng G, Song J. Effects of periodontal endoscopy on the treatment of periodontitis: A systematic review and meta-analysis. J Am Dent Assoc. 2017;148:750–759.
- Harrel SK, Nunn ME, Abraham CM, Rivera-Hidalgo F, Shulman JD, Tunnell JC. Videoscope assisted minimally invasive surgery (VMIS): 36-month results. J Periodontol. 2017;88:528–535.
- Drisko CL, Killoy WJ. Scaling and root planing: Removal of calculus and subgingival organisms. Curr Opin Dent. 1991;1:74–80.
- Drisko CL, Cochran DL, Blieden T, et al. Position paper: sonic and ultrasonic scalers in periodontics. Research, Science and Therapy committee of the American Academy of Periodontology. J Periodontol. 2000;71:1792–1801.
- Rethman M. Open forum digest. AAP Connect. October 3, 2019.
This information originally appeared in Rethman MP, Cobb CM, Sottosanti JS, Sheldon LN, Harrel SK. Scaling and root planing remain key to successful periodontal therapy. Decisions in Dentistry. 2021;7(9):25-31.


