 TefiM / iStock / Getty Images Plus
TefiM / iStock / Getty Images Plus
Ensuring Access During Implant Placement
Innovative digital technological advancements have improved access to the alveolar bone during implant placement.
Innovative digital technological advancements, such as guided computer-assisted surgery, have improved implant placement by substantially increasing the precision with which implants are positioned for optimal biological and prosthetic locations.1,2 Effective access to the alveolar bone is a crucial step in the implant-placement process.
Conventional approaches to dental implant insertion require crestal incision and mucoperiosteal flap reflection to ensure visual recognition of underlying anatomical landmarks, such as foramina, lingual undercuts, and maxillary sinuses; prevent injury to the patient; and support proper placement of the implant for long-term success.3
Despite its potential benefits, flapless surgery is often regarded as unperceptive due to difficulties in assessing the shape and health of underlying alveolar bone and anatomical regions.4 However, with the use of CBCT and dental implant planning software, the residual bone and essential anatomical features in surgery sites may be precisely analyzed via three-dimensional radiography.
The use of CBCT-guided surgery permits advanced detection of vestibular concavities and lingual-palatal bone plates around the desired recipient site, thereby optimizing bur angulation and decreasing the likelihood of bone perforations and fenestrations.5,6
CBCT scans assist with planning and visualizing the placement by creating a surgical drilling guide.5 The use of traditional dental X-rays for implant insertion is no longer an accepted practice due to the considerable risk involved and limited diagnostic ability of anatomical accuracy.7
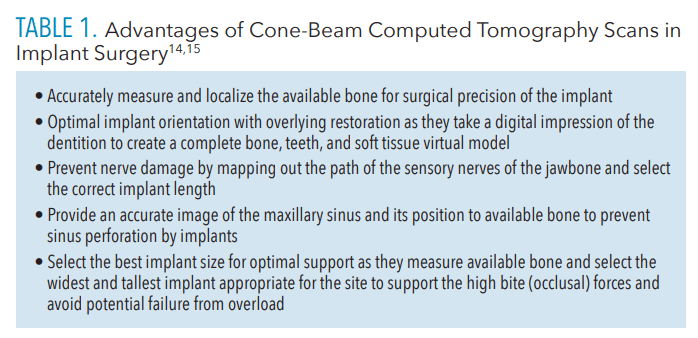
Although some oral specialists still rely on two-dimensional panoramic imaging for routine cases, the American Academy of Oral and Maxillofacial Radiology recommends the use of cross-sectional imaging for all dental implant surgeries as the evidence demonstrates that CBCT offers significant advantages that can alter treatment planning and improve surgical outcomes (Table 1).8
References
- Naeini EN, Atashkadeh M, De Bruyn H, D’Haese J. Narrative review regarding the applicability, accuracy, and clinical outcome of flapless implant surgery with or without computer guidance. Clin Implant Dent Relat Res. 2020;22:454–467.
- Romandini M, Ruales-Carrera E, Sadilina S, Hämmerle CHF, Sanz M. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontol 2000.2022;10:1111.
- Yadav MK, Verma UP, Parikh H, Dixit M. Minimally invasive transgingival implant therapy: a literature review. Natl J Maxillofac Surg. 2018;9:117–122.
- Cai H, Liang X, Sun DY, Chen JY. Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation: a systematic review and meta-analysis. World J Clin Cases. 2020;8:1087–1103.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS One.2014;9:e100624.
- Nkenke E, Vairaktaris E, Bauersachs A, et al. Acceptance of virtual dental implant planning software in an undergraduate curriculum: a pilot study. BMC Med Educ. 2012;12:90.
- Gupta J, Ali SP. Cone-beam computed tomography in oral implants. Natl J Maxillofac Surg.2013;4:2-6.
- Weiss R 2nd, Read-Fuller A. Cone-beam computed tomography in oral and maxillofacial surgery: an evidence-based review. Dent J (Basel).2019;7:52.
This information originally appeared in Monchik C, Marsh I. Innovations in implant therapy. Dimensions of Dental Hygiene. 2023;21(3)34-37.


