
Tobacco Intervention Strategies
An effective approach to prevention and cessation counseling will help address the growing prevalence of tobacco use among young people.
This course was published in the December 2017 issue and expires December 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
- Explain the various alternative tobacco products and prevalence of use.
- Describe the health effects of tobacco use.
- Discuss the “5 A’s” of tobacco cessation, and the approach to addressing these with patients.
- Summarize resources available to assist with tobacco cessation intervention.
The U.S. Surgeon General refers to tobacco use as a pediatric disease because 90% of adult tobacco users start the habit before they turn 18.1 This is a concern because tobacco use appears to be on the rise in young people. At least in part, this increase may be due to the advent of alternative tobacco products (ATPs) ranging from hookah pipes to electronic cigarettes (e-cigarettes). Amrock and Wietzman2 have characterized the use of ATPs as the “second front in the war on tobacco.”
Cigarettes are the most commonly used form of tobacco among adults.3 The prevalence of tobacco use among adults and youth in the United States is measured by national surveys, which reveal 17% of adults, 9% of high school students and 2% of middle school students are cigarette smokers (defined as smoking > 1 cigarette per day in the past 30 days).3,4 This is misleading, however, because young people tend to favor ATPs.3,4 In terms of the overall prevalence of tobacco use, Singh et al5 report that approximately 7% of middle school students, 25% of high school students and 21% of adults use tobacco products. These include smoked and smokeless items, such as cigars, snus, dissolvables and chewing tobacco, to name a few.6,7 Electronic nicotine delivery systems (ENDS) heat liquid containing nicotine to an aerosol that is inhaled;8 ENDS include vaporizers, vape pens, hookah pens, e-pipes and e-cigarettes. According to the U.S. Surgeon General, these delivery systems can also be used for cannabinoids and other drugs.9,10
The increased use of ENDS by youth is occurring more rapid than in adults, with national surveys showing 1% to 5% of adults using ENDS, compared to 14% to 16% of high school students.4,5,11 From 2011 to 2015, the use of ENDS among high school students increased from 1.5% to 16%; in middle school students, the reported use increased from < 1% to more than 5% in the same time period.5 Even more alarming is that approximately 10% of high school and 8% of middle school students report daily use of ENDS.4 Among those using e-cigarettes, 63% report using flavored ENDS products, suggesting this enhances their appeal to adolescents.4,9 In addition, ENDS use is also associated with the utilization of other tobacco products among youth and young adults.9,11
The Tobacco Products and Risk Perceptions Survey found that 1% of adults who had never smoked reported using ENDS in the past 30 days, with almost 5% of those who had never smoked using these products at some point.12 It is concerning that individuals who identify as nonsmokers are using ENDS, suggesting a widespread belief they are less harmful than other tobacco products.9 The survey also found nearly 21% of current smokers reported using ENDS.12 Although systematic reviews of ENDS use to reduce the harmful effects of cigarette smoking and decrease smoking frequency suggest ENDS may be helpful in tobacco cessation,13,14 the long-term safety and health effects of ENDS use are unknown. Additionally, the evidence about the ability of ENDS to reduce smoking is of low quality.13,14 Oral health professionals should monitor emerging information on this topic and be wary of e-cigarette vendors wanting to advertise their products in the dental office.
Hookah tobacco is known by a number of names, including water pipe tobacco, maassel, shisha, narghile and argileh.15 Hookah pipes tend to be used socially at parties, cafes and lounges.16 Flavor enhancers may also be added, and almost 79% of youth who used a hookah reported choosing it because of the flavors available.17 Many users believe hookah smoking is less harmful than cigarettes, but evidence suggests the health outcomes and addiction issues are similar.18 Water pipe smoking sessions tend to last 30 to 90 minutes. A systematic review and meta-analysis found one session of hookah smoking resulted in 74.1 liters of smoke inhalation versus 0.6 liters for smoking a cigarette.19 Higher levels of carbon monoxide, nicotine and tar are also released during a hookah session.
Although the prevalence of water pipe use among adults is approximately 4%,3 prevalence among youth is higher. About 7% of high school students report hookah use, an increase from 4% in 2011.5 Among middle school students, the prevalence of hookah use increased from 1% in 2011 to 2% in 2015.5
Smokeless tobacco products include chewing tobacco (also known as spit tobacco), dry snuff, and moist snuff or snus. These products contain high-intensity sweeteners, such as sucralose, in higher concentrations than is found in candy and soda.20 Sweeteners mask the unpleasant taste of tobacco and make it more appealing, especially to youth.20 In 2014, 59% of youth who used smokeless tobacco reported choosing a flavored variety.21
About 2.5% of adults report using smokeless tobacco products;3 however, 6% of high school students and almost 2% of middle school students report using smokeless tobacco.5 The percentage of youth using smokeless tobacco decreased about 1% between 2011 to 2015.5 Despite this decrease, frequent use (defined as > 20 days in the last 30 days) of smokeless tobacco was most prevalent among high school students (42%) and middle school students (29.2%).4
Dissolvable tobacco come in strips (placed on the tongue to dissolve), sticks (similar to large toothpicks), and lozenges or orbs.22 The nicotine content varies, but these products can contain as much or more than a typical cigarette. Data on the prevalence of dissolvable tobacco use are not available because it is typically combined with smokeless tobacco in national surveys.
Cigars, little cigars and cigarillos, as well as tobacco wrapped in a tobacco leaf, are additional forms of tobacco use.23 One cigar contains as much tobacco as a pack of cigarettes.23 Little cigars and cigarillos may be flavored to enhance appeal, especially to youth and young adults. Adolescents reported using cigars because they liked the flavors (73.8%) and considered them affordable (58.2%).17 In the study by Singh et al,5 approximately 9% of high school students and 5% of adults reported using cigars in the past 30 days.
HEALTH EFFECTS
In addition to the well-known negative health effects of tobacco use, nicotine exposure significantly harms the developing adolescent brain.9 The fact that use of ATPs among youth is increasing emphasizes the need for effective prevention and cessation programs.
Like traditional cigarette smoking, hookah smoking harms cardiovascular and respiratory health by increasing blood pressure, decreasing immunity, and raising the risk for chronic obstructive pulmonary disease.18,24 A systematic literature review found five studies that evaluated the association between periodontal disease and hookah smoking.24 Of these studies, four were with the same participants, limiting the sample size. This led Waziry et al24 to suggest that it is unclear whether an association exists between water pipe smoking and periodontal disease. The health effects of heated and aerosolized components of e-cigarette liquids (e.g., nicotine, solvents, flavoring and toxicants) are unknown at this time.9
Another emerging trend is polytobacco use, or the use of more than one type of tobacco product. Polytobacco use is increasing among those who use ATPs and is associated with increased risk of nicotine addiction.25,26 This addiction leads to more problems with tobacco dependence and can hinder the success of tobacco cessation efforts.25,26 Thus, the long-term health effects of polytobacco use warrant further research.
PREVENTION AND CESSATION
Tobacco prevention and cessation programs have been focused on smoking, leaving few resources to address ATPs. According to the U.S. Preventive Services Task Force’s (USPSTF) guidelines for children and adolescents, efforts should focus on assessing risk, interventions to prevent tobacco use, and tobacco cessation.27 Risk assessment should include exposure to parental smoking, access to tobacco products, peers who use tobacco, and exposure to tobacco advertising.27
Oral health professionals can provide preventive messages about tobacco use that address oral and systemic health. Messages need to be meaningful for youth in order to make a difference. Highlighting the short-term effects of tobacco use, such as staining of teeth, breath malodor or shortness of breath — which may impact endurance during athletic events — may be an effective stratagem when addressing young tobacco users. According to the USPSTF, however, there is limited evidence related to the most effective approach to tobacco cessation in youth, and there are no pharmaceutical agents approved for this age group.27
Current USPSTF guidelines for adults continue to recommend the “5 A’s” framework for tobacco intervention: asking about tobacco use; advising tobacco users to quit; assessing readiness to quit; assisting with quitting; and arranging follow-up.28 A modified version focused on ask, advise, and refer has also been proposed for oral health professionals, but research suggests patients are more successful in quit attempts when using the “5 A’s” approach.29
Screening patients for tobacco use, including ATPs, may be more challenging than for more traditional cigarette or smokeless tobacco products, because ATPs are not normally included on the medical history. Considering that individuals who report never using tobacco may, in fact, use ENDS, clinicians should takes steps to gather comprehensive information.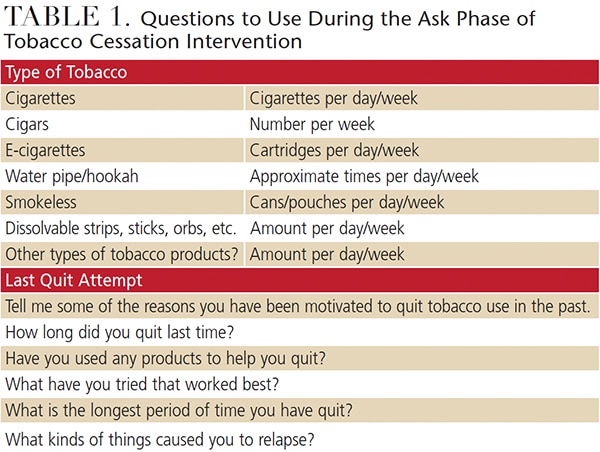
Ask. The health history should list the actual types of ATPs to prompt questions by the oral health professional about the various types of tobacco products and frequency of use. Table 1 provides a sample of the information needed for tobacco use assessment.
Advise. Providers should advise patients to quit tobacco as a means of supporting oral and systemic health. Patients should be educated about cessation efforts in clear language that is personalized according to the individual’s needs at each appointment.30 Clinicians should expect ambivalence (conflicted feelings about tobacco use) and listen nonjudgmentally to the patient’s concerns about tobacco cessation.
Assess. Oral health professionals are advised to assess patients’ readiness to quit tobacco use. This readiness to change behavior is a component of the Transtheoretical Model of Behavior Change, which is foundational to motivational interviewing and is widely used to help patients quit smoking.31 In motivational interviewing, oral health professionals act as guides to assist patients in choosing to change behavior and support self-efficacy. While an in-depth discussion of motivational interviewing is beyond the scope of this article, many resources are available on this topic.
Patients may be in various stages of quitting, including precontemplation (not interested in quitting), contemplation (thinking about quitting), preparation (planning to quit in the next 30 days), action (quitting successfully for up to six months), and maintenance (quitting successfully for more than six months). The stage of readiness to quit should also be recorded in the patient’s chart.
Assist. Table 2 provides a sampling of tobacco cessation resources. The resources for clinicians provide information on behavioral and pharmacologic approaches to assist patients in tobacco cessation. If the office or clinic has a website, links can be provided for tobacco cessation resources. Given the time constraints and expertise of the dental team, ideally, collaboration by an interprofessional team to assist patients in successfully quitting tobacco is the preferred approach. The team may include the patient’s physician, nurse practitioner, physician assistant, pharmacist and/or substance abuse counselor, as well as others. Oral health professionals should bear in mind that even individuals who smoke only one cigarette per day have a 64% higher risk of early death (primarily from lung cancer) than never smokers.32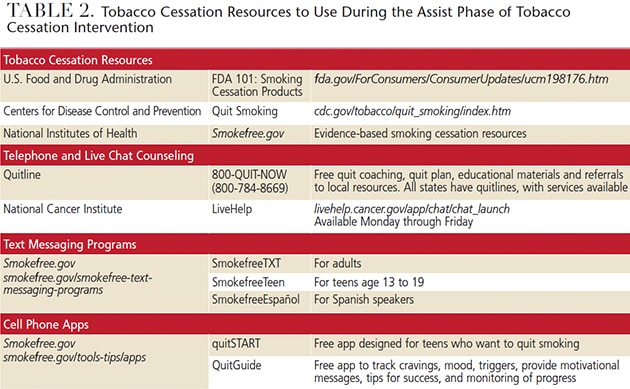
Arrange. Clinicians should follow up with patients a week after a planned quit date, as well as at each recare appointment, to reassess or provide support for another quit attempt or relapse prevention.30 In 2006, approximately 44% of adults reported a quit attempt in the past year, yet, without formal treatment, 95% to 98% resumed tobacco use. This underscores the need for oral health professionals to be actively involved in relapse prevention,33 which involves sharing strategies to help patients avoid or recover from lapses or relapses. Avoiding blame and guilt for a relapse is essential because negative emotions reduce the chances of success.33 Patients should be encouraged to examine the relapse to identify the trigger(s) and find approaches to avoid or overcome these trigger(s).33
CONCLUSION
Although tobacco use is declining in adults, it is on the rise in youth. The use of ATPs by young patients is particularly concerning. Considering that tobacco use in adulthood generally begins in adolescence, oral health professionals are ideally positioned to offer preventive messages to middle and high school students. Such educational messages can have a lasting impact and prevent tobacco use into adulthood. The health implications of tobacco use, including ATPs, are serious. By intervening to prevent and reduce its use, oral health professionals can help patients avoid preventable disease.
REFERENCES
- U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress, 2014. A Report of the Surgeon General. Available at: surgeongeneral.gov/library/reports/50-years-of-progress. Accessed November 7, 2017.
- Amrock SM, Weitzman M. Alternative tobacco products as a second front in the war on tobacco. JAMA. 2015;314:1507–1508.
- Hu SS, Neff L, Agaku IT, et al. Tobacco product use among adults — United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65:685–691.
- Neff LJ, Arrazola RA, Caraballo RS, et al. Frequency of tobacco use among middle and high school students — United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:1061–1065.
- Singh T, Arrazola RA, Corey CG, et al. Tobacco use among middle and high school students — United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65:361–367.
- Lauterstein D, Hoshino R, Gordon T, Watkins BX, Weitzman M, Zelikoff J. The changing face of tobacco use among United States youth. Curr Drug Abuse Rev. 2014;7:29–43.
- McMillen R, Maduka J, Winickoff J. Use of emerging tobacco products in the United States. J Environ Public Health. 2012;2012:1–8.
- U.S. Food and Drug Administration. Vapes, E-Cigarettes,Hookah Pens, and other Electronic Nicotine Delivery Systems (ENDS). Available at: fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm456610.htm. Accessed November 7, 2017.
- U.S. Department of Health and Human Services. E-cigarette Use Among Youth and Young Adults: A Report of the Surgeon General — Executive Summary. Available at: e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Exec_Summ_508.pdf. Accessed November 7, 2017.
- Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136:611–616.
- Gilreath TD, Leventhal A, Barrington-Trimis JL, et al. Patterns of alternative tobacco product use: emergence of hookah and e-cigarettes as preferred products amongst youth. J Adolesc Health. 2016;58:181–185.
- Weaver SR, Majeed BA, Pechacek TF, Nyman AL, Gregory KR, Eriksen MP. Use of electronic nicotine delivery systems and other tobacco products among USA adults, 2014: results from a national survey. Int J Public Health. 2016;61:177–188.
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. September 14, 2016. Epub ahead of print.
- Glasser AM, Collins L, Pearson JL, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med. 2016;52:e33–e66.
- U.S. Food and Drug Administration. Hookah Tobacco (Shisha or Waterpipe Tobacco). Available at: fda.gov/TobaccoProducts/Labeling/ ProductsIngredientsComponents/ucm482575.htm. Accessed November 7, 2017.
- Maziak W, Taleb ZB, Bahelah R, et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl 1):i3–i12.
- Ambrose BK, Day HR, Rostron B, et al. Flavored tobacco product use among U.S. youth aged 12–17 Years, 2013–2014. JAMA. 2015;314:1871–1873.
- Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A systematic review of effects of waterpipe smoking on cardiovascular and respiratory health outcomes. Tob Use Insights. 2016;9:13–28.
- Primack BA, Carroll MV, Weiss PM, et al. Systematic review and meta-analysis of inhaled toxicants from waterpipe and cigarette smoking. Public Health Rep. 2016;131:76–85.
- Miao S, Beach ES, Sommer TJ, Zimmerman JB, Jordt SE. High-intensity sweeteners in alternative tobacco products. Nicotine Tob Res. 2016;18:2169–2173.
- Corey CG, Ambrose BK, Apelberg BJ, King BA. Flavored tobacco product use among middle and high school students — United States, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:1066–1070.
- U.S. Food and Drug Administration. Tobacco Products: Dissolvable Tobacco Products. Available at: www.fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm482569.htm. Accessed November 7, 2017.
- U.S. Food and Drug Administration. Tobacco Products: Cigars, cigarillos, little filtered cigars. Available at: www.fda.gov/TobaccoProducts/ Labeling/ProductsIngredientsComponents/ucm482562.htm. Accessed November 7, 2017.
- Waziry R, Jawad M, Ballout RA, Al Akel M, Akl EA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2016. Epub ahead of print.
- Sung HY, Wang Y, Yao T, Lightwood J, Max W. Polytobacco use of cigarettes, cigars, chewing tobacco, and snuff among U.S. adults. Nicotine Tob Res. 2016;18:817–826.
- Butler KM, Ickes MJ, Rayens MK, Wiggins AT, Hahn EJ. Polytobacco use among college students. Nicotine Tob Res. 2016;18:163–169.
- Moyer VA, U.S. Preventive Services Task Force. Primary care interventions to prevent tobacco use in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:552–557.
- Siu AL, U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:622–634.
- Gordon JS, Andrews JA, Crews KM, Payne TJ, Severson HH. The 5A’s vs 3A’s plus proactive quitline referral in private practice dental offices: preliminary results. Tob Control. 2007;16:285–288.
- Black JH 3rd. Evidence base and strategies for successful smoking cessation. J Vasc Surg. 2010;51:1529–1537.
- Lindson-Hawley N, Thompson TP, Begh R. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2015:CD006936.
- Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the National Institutes of Health — AARP diet and health study. JAMA Intern Med. 2017;177:87–95.
- Collins SE, Witkiewitz K, Kirouac M, Marlatt GA. Preventing relapse following smoking cessation. Curr Cardiovasc Risk Rep. 2010;4:421–428.
FEATURED IMAGE BY NICOLASMCCOMBER/E+/GETTY IMAGES PLUS
From Decisions in Dentistry. December 2017;3(12):44—47.





[…] Read more about tobacco intervention strategies here: https://decisionsindentistry.com/article/tobacco-intervention-strategies/ […]
[…] importance of selecting healthy foods are made to the lower grades, while lessons on prevention and strategies for tobacco cessation are delivered to students in the higher […]