
Using Evidence to Make Informed Decisions
Citing ergonomics as an example, this article examines the steps involved in evidence-based decision-making.
steps involved in evidence-based decision-making.
The author has no commercial conflicts of interest to disclose.
This 2 credit hour self-study activity is electronically mediated.
Objectives
After reading this course, the participant should be able to:
- Define evidence-based dentistry as it applies to ergonomics.
- Describe the steps used in the practice of evidence-based dentistry.
- Determine if an article provides the best evidence through consideration of its research design.
- Evaluate the value of an article through the application of key statistical results.
Ergonomics is often used to reduce or prevent musculoskeletal disorders, which are common among oral health professionals. On average, 66% of dental practitioners experience musculoskeletal pain at some point during their careers.5 Oral health professionals may be taught how to safely and effectively position themselves and patients through the principles of ergonomics. But how often do practitioners’ behaviors change when new ergonomic evidence or equipment is introduced? The practice of EBD can be applied in this situation.
Improving performance and minimizing the level of experience required to develop sound clinical judgment are just some of the advantages of EBD. Yet barriers exist to implementation, including a lack of time to search and read; the need to develop new skills (e.g., efficient search skills, critical appraisal, and statistical understanding to interpret the results); and the lack of generalizability of research that offers summaries and/or guidelines based upon current literature.6 Even when such information is located, practitioners should always ask, “Is the interpretation and recommendation based upon the best possible evidence for my practice?“ In articles reporting the results of a single study, the authors rarely make clinical recommendations — that is left up to the reader. As such, oral health professionals need to be able to evaluate research within an EBD framework.
An evidence-centered approach to clinical decision-making is based upon the application of scientific research, working clinical expertise and the patient’s values and expectations.7 When it comes to ergonomic choices, the dental practitioner is the “patient,” trying to prevent, reduce or eliminate musculoskeletal problems that may develop or have developed due to practice. There are five steps to the evidence-based process.
STEP 1: DEVELOP A QUESTION
The purpose of writing a question is to help narrow the scope of the search. The strategy for writing the question is PICO based (Person, Intervention, Comparison and Outcome). “Person” refers to the patient’s or population’s characteristics, including a description of the problem. “Intervention” speaks to the patient management technique being implemented, such as the use of equipment. In ergonomics, new instruments and techniques adopted by the clinician to reduce the strain on his or her musculoskeletal health serve as intervention. “Outcome” is focused on how well the intervention alleviated the sign or symptom during or after the clinical task.
Note there is not always a need for the “comparison” step. In the sidebar example, the comparison line could have been left empty, which would indicate the clinician is only interested in learning about lightweight instruments. Each part of PICO provides keywords that can be used in a literature search to support efficacy. Using PICO helps clinicians formulate an answerable clinical question.
STEP 2: EVIDENCE SEARCH
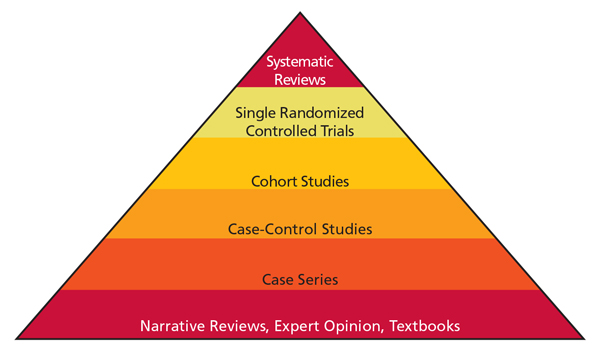
The next step is to search for the best possible evidence. There are different types of evidence, based on research design. The evidence-based pyramid demonstrates the hierarchy of information (Figure 1). The higher levels of the pyramid represent the most likely sources of high-quality research. Systematic reviews are at the top of the pyramid because they often overcome many limitations of single studies. By providing comprehensive analyses, systematic reviews summarize the available research and offer recommendations for practice. The strength of a systematic review depends on the level and amount of research that is currently available. In regard to patient management techniques, the best possible systematic review is composed of randomized controlled trials (RCT). Systematic reviews, however, are not always available. The next level of evidence is a single-study RCT.
An evidence search begins by plugging the search or keywords determined by PICO into an electronic database (such as PubMed, Dentistry and Oral Sciences Source, and EBSCOhost). To find evidence, it’s important to develop quality search skills. The best place to begin is PubMed (pubmed.gov), a free search engine developed by the U.S. National Library of Medicine and National Center for Biotechnology Information. The PubMed Clinical Queries tool can be used to locate all available research. Using keywords overcomes the barrier of time needed to search. Additional search strategies can be found in the tutorials provided at the PubMed site.
STEP 3: APPRAISE THE EVIDENCE
Appraising the research gathered during Step 2 for quality and applicability begins with reading the title and abstract, which will determine the article’s relevance to the clinical question (PICO). The next factor that needs to be determined is the study’s internal validity.8 Internal validity refers to how well a research study is conducted, and can be established by answering three questions.
- Have subjects been assigned to groups randomly?
- Were the investigators as well as the subjects blinded?
- Were there few dropouts?
Randomization is considered the most robust method for reducing bias because it helps to create the most homogeneous treatment groups.8 When subjects and investigators are blinded, they are unaware of which subjects are using which intervention. This reduces the risk of bias if investigators or subjects are hoping for specific outcomes. Computerized randomization that is concealed from investigators is one of the best methods of randomizing and blinding subjects and investigators. A study in which at least 85% of its participants complete the study is the benchmark.8 A study demonstrates good internal validity when these three criteria are met. While this is a quick way to determine the strength (or internal validity) of a research design, a more in-depth discussion is available in Evidence-Based Decision Making: a Translational Guide for Dental Professionals.8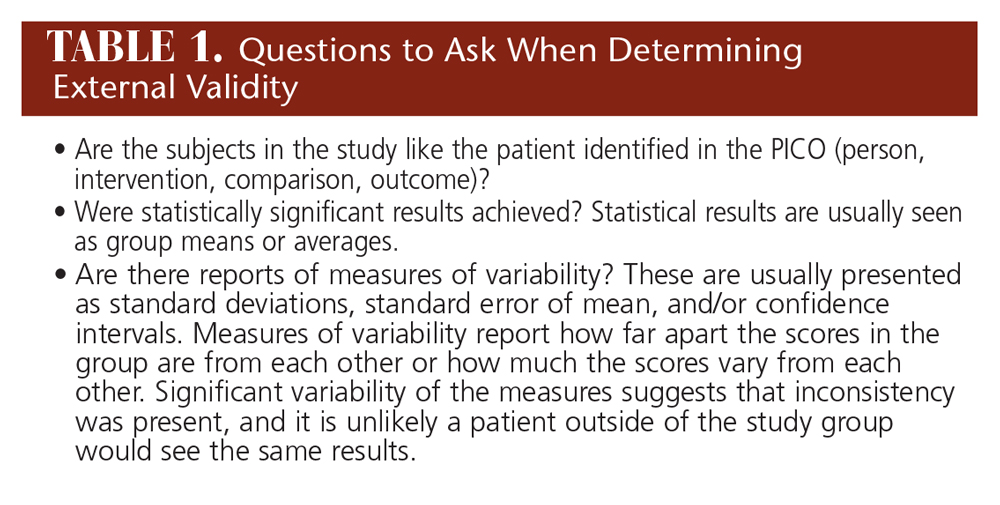
External validity is determined by how useful the information is to the patient and different areas of practice. External validity is based on how applicable the research is beyond the sample subjects. This is established by understanding who the subjects are, evaluating the statistical results, and noting whether the research occurred in different real-world settings. Table 1 includes some questions to ask when determining external validity.
Individuals who are impacted by the treatment are usually most interested in its positive effects. Achieving a meaningful measure and then showing a positive result make the results important to patients. The p value demonstrates whether the results of each group in a study were different at the end of treatment. A p value less than 0.05 means the difference did not occur by chance. Results should also indicate how large the difference is between groups (this is called the effect size of the difference). In other words, is the effect of treatment significant enough to make a difference that is easily seen or felt, thus providing a significant impact in day-to-day practice?
STEPS 4 AND 5: APPLY AND EVALUATE RESULTS
The fourth step is to apply the intervention to the patient, giving it the appropriate amount of time in order to accurately determine results. Evaluating whether the findings are relevant to the patient, problem, or question is key to successful application.11
The final step is to assess the process, the clinician’s performance and the outcomes of the intervention. This can include evaluating the outcomes relative to the health and function of the patient, patient satisfaction, and input into the decision-making process — as well as an examination of the EBD process itself.11
CONCLUSION
Embracing the EBD model is essential to making improvements in patient management, just as proper ergonomics is key to maintaining clinicians’ health. But though ergonomic principles have been developed, they often are not adequately used to make beneficial practice changes. By learning the steps of EBD, dentists can hone their search skills and develop a deeper understanding of the results cited in high-quality studies. As the foregoing demonstrates, EBD may also help clinicians evaluate ergonomic interventions, enabling them to make the best decisions based on solid evidence.
SIDEBAR: EVIDENCE-BASED DENTISTRY IN ACTION
A dentist employs a dental hygienist who has developed consistent arm pain in her dominant arm that is not alleviated with rest. In discussing the issue, it’s decided the best approach is to find an effective intervention that may eliminate the need for invasive treatment. The dentist suggests that using a different piece of equipment may help. Before the employee commits to a purchase, however, the pair want to know how strong the recommendation would be to change equipment.
Step 2. She uses PubMed to locate any related systematic reviews. After typing in the keywords dental hygienist AND arm pain AND instruments, one article is located, but no systematic reviews are found.
Step 3. The article is “The Effects of Periodontal Curette Handle Weight and Diameter on Arm Pain: A Four-Month Randomized Controlled Trial.”9 The title reveals that the study is an experimental research design that is high on the evidence-hierarchy pyramid. The abstract discloses that dental hygienists with arm pain are the subjects, and they experienced significant improvement in pain scores for the shoulder region when lightweight instruments were used. Before the clinician decides to switch instruments, however, further interpretation of the study design and results is needed.
In this study, the subjects were randomly assigned to one of two groups, with each group using an instrument of specific weight and diameter. The subjects and investigators were blinded. The completion rate was 95% (only five subjects discontinued using the intervention).
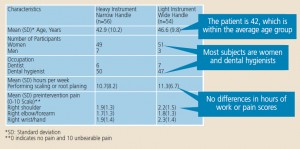
Applying this information about external validity to the patient in the scenario starts with the question: Does the patient from the PICO qualify for the study? Reviewing the modified table (Figure 2) provides characteristics of the subjects at a glance, and answers the question, “Is the patient similar or too different for the results to apply?” The clinician falls within the age range of subjects in the study, and also matches the mean hours per week and measure of pain that was noted preintervention.
Where the subjects differ is in their reports on the exit survey, in which higher ratings were obtained for the light instrument with wide handle. From these means (standard deviation or SD), a secondary outcome, the effect of the size of each group, can be calculated by dividing the mean change by the SD for the change (Figure 3). The interpretation of these results implies minimal negative effect for the heavy-handle group, and moderate positive effect for the light-handle groups.10 So before the treatment begins and while the treatment is ongoing, the dental professionals did not differ in their daily tasks; the only difference was the instrument they were using. After completing the study, statistical difference was noted in favor of the light-handle group with strong internal validity. The external validity or generalizability comes from the experiment being carried out in various dental clinics and not in one laboratory setting, and the likelihood of finding the same outcome among individuals with similar characteristics.
What characteristics might best describe the individual most likely to benefit? A general linear model (Figure 4) is one way to predict outcomes in the future.

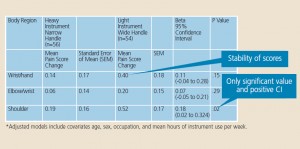
In this study, the adjusted models included age, sex, occupation, and mean hours of instrument use per week. Specifically, it determines if the amount of change in pain can be predicted based on the instrument size and weight. It creates a model for future prediction. Figure 4 provides mean pain score changes with standard error of the mean (SEM) for the two groups, and the results of the regression analyses for different aspects of the upper extremity. The SEM is the SD related to taking measures repeatedly. The SEM means that the scores are reliable — less than one has very small variations.
The only significant model found is the relationship between change in pain scores and pain in the shoulder. Beta coefficient means the amount of change in the dependent variable of pain that is expected if the new instrument is put into use. The confidence interval (CI) for beta means 95% surety that the true value for beta is between 0.020 and 0.324. While the model is significant, the change is very little: 0.180. Using the 95% CI, this change could be as small as 0.020 or as large as 0.324. While the lightand wide-diameter instrument changed the pain experienced in the shoulder for those individuals who used it, the effect of size was considered modest and the pain was not completely eliminated. Because the treatment was effective, the next choice is to decide if the amount of change is enough to warrant the use of a new piece of equipment.
Step 4 and Step 5. As this was a four-month study, the clinician must give the intervention at least this much time to work. If the time is cut short and the treatment does not alleviate her pain, it will be unclear whether the new instrument was the problem or if the treatment was not given enough time to achieve results.
REFERENCES
- McGlone P, Watt R, Sheiham A. Evidence-based dentistry: an overview of the challenges in changing professional practice. Br Dent J. 2001;190:636–639.
- American Dental Association. Policy on Evidence-Based Dentistry. Available at: www.ada.org/en/about-the-ada/ada-positions-policies-and-statements/policy-on-evidence-based-dentistry. Accessed September 10, 2015.
- American Dental Association. Evidence-Based Dentistry. Available at: ada.org/en/science-research/evidence-based-dentistry. Accessed
September 10, 2015. - International Ergonomics Association. Definition and Domains of Ergonomics. Available at: www.iea.cc/whats/index.html. Accessed September 10, 2015.
- Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry: strategies to address the mechanisms leading to musculoskeletal disorders. J Am Dent Assoc. 2003;134:1604–1612.
- Madhavji A, Araujo EA, Kim KB, Buschang PH. The attitudes, awareness, and barriers towards evidence-based practice in orthodontics. Am J Orthod Dentofac. 2011; 140(3):309–316.
- Straus SE, Richardson WS, Glasziou P, Haynes RB. Evidence-based Medicine: How to Practice and Teach EBM. 3rd ed. New York: Elsevier, 2005.
- Forrest JL, Miller SA, Overman P, Newman MG. Evidence-Based Decision Making: A Translational Guide for Dental Professionals. Baltimore: Lippincott Williams & Wilkins, 2008.
- Rempel D, Lee DL, Dawson K, Loomer P. The effects of periodontal curette handle weight and diameter on arm pain. A four-month randomized controlled trial. J Am Dent Assoc. 2012;143(10):1105–1113.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences, 2nd Ed. Hillsdale: Lawrence Erlbaum, 1988.
- Forrest JL, Miller SA. Evidence-based decision making. Dimensions of Dental Hygiene. 2005;3(9):12.





[…] knowledge gaps on this topic, the team emphasizes that deciding which ergonomic interventions are most beneficial to a clinician or practice is imperative, as MSDs contribute to burnout, poor […]