
Silver Diamine Fluoride Use in Older Adults
This agent shows promise for prevention and caries arrest in geriatric patients.
PURCHASE COURSE
This course was published in the August 2016 issue and expires 08/31/19. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Explain the indications and contraindications for silver diamine fluoride (SDF), as well as the evidence for its efficacy in treating caries in the roots and crowns of older adults.
- Safely apply SDF, and supervise auxiliaries applying the agent, and evaluate whether treatment is successful.
- Discuss the precautions in handling SDF in order to protect patients, staff and the clinic environment.
Older adults are generally more susceptible to tooth decay than younger patients.1 Medical complexity, physical frailty, psychological barriers and financial limitations commonly challenge caries management in this population. In combination with more older adults retaining their natural dentition, the rapid growth of the 65-and-older cohort is further taxing the U.S. oral health care system. In addition, systemic diseases, such as diabetes, and salivary dysfunction, including Sjögren syndrome and xerostomia (Figure 1), further complicate the clinical picture.1 Strategies that increase access and improve outcomes for older adults are needed. This paper will address silver diamine fluoride (SDF), an agent that provides U.S. clinicians with an additional treatment modality that can help accomplish these goals.
Data show that a growing number of older adults are visiting the dentist. The percentage of older adults with at least one visit annually increased from 38% in 2000 to 42% in 2011, for example, while visits by adults ages 19 to 64 decreased from a peak of 41% in 2003 to 36% in 2011.2 According to data from the U.S. Medical Expenditure Panel Survey, nearly 70% of privately insured older adults sought dental care. This substantially exceeds the rate among privately insured younger adults. Compared to a younger patient, the older adult also presents with more tooth surfaces that are prone to decay. Although complete tooth loss has dropped to less than half of what it was in the 1950s, gingival recession, untreated decay and periodontal disease are common.3 Root dentin exposed from recession demineralizes at a less acidic pH than enamel, further increasing caries risk. A systematic review noted that 24% of older adults have untreated root caries.4 Compounding these issues, today’s older adults are much less willing to have compromised teeth extracted than previous generations.1
The patterns of disease for older adults also vary from those seen in younger individuals. A significant portion of tooth decay is recurrent disease associated with failing restorations. In fact, the majority of tooth decay in older adults is restoration failure at the gingival margin (Figure 2).5 These lesions can be difficult to diagnose and restore.1 No materials have been shown to provide consistent long-term results, even when they contain and release fluoride. Although glass ionomers provide some benefit over composites in the xerostomic population, new lesions continue to develop.6
There is a strong association between general health and oral health, with chronic conditions — and the medications used to manage them — increasing the risk of dental and periodontal problems. In light of the oral/systemic connection, improvements in the oral health of older adults may offer some level of protection against systemic diseases, including pneumonia.3 Clearly, oral health care for older adults would benefit from a noninvasive, safe approach to preventing and arresting caries.
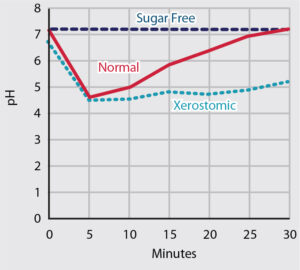
UNPUBLISHED DATA, COURTESY JOHN D.B. FEATHERSTONE, PhD
Aqueous silver has been used to treat tooth decay in the U.S. for more than a century. The founders of modern dentistry commonly used silver nitrate. In the last 20 years, dental researchers have more rigorously assessed the efficacy and safety of SDF. In the 1960s, SDF was created as an improvement to silver nitrate, and approved by Japan’s Ministry of Health. Although widely used in other countries, the first SDF product cleared by the U.S. Food and Drug Administration became available in 2015. This is a colorless topical medicament containing 25% (w/v) silver, 8% ammonia and 5% fluoride.7 The silver acts as an antimicrobial, the fluoride promotes remineralization, and the ammonia stabilizes high concentrations in solution.8 Application involves drying the surface, and applying sparing amounts of the liquid to the tooth, with no special instructions for post application care. A layer of petroleum jelly can be placed to protect the gingiva prior to application in cervical areas. Treated lesions will discolor to black over the next week (Figure 3), and the lesions will harden.
To systematically review the evidence, a literature review was designed to search PubMed with the following search terms: ‘“33040-28-7” OR “1Z00ZK3E66” OR “SDF” OR “silver fluoride” OR “silver diammine fluoride” OR “diammine silver fluoride” OR “ammonical silver fluoride” OR “ammoniacal silver fluoride.” The review turned up 12 published randomized clinical trials of at least 12 months duration that evaluated SDF for caries arrest and/or prevention, including studies that addressed root caries and focused on lesions in older adults.9,10 Two case studies document profound efficacy for treating severe caries resulting from chemo-radiation-therapy-induced xerostomia.11,12

COURTESY STEVE DUFFIN, DDS

COURTESY STEVE DUFFIN, DDS
USE IN OLDER ADULTS
Six large randomized clinical trials demonstrated better caries prevention with SDF than any other noninvasive material except sealants, and nine demonstrated better caries arrest than any other noninvasive material (three studies overlap in evaluating both prevention and arrest).13 This material’s performance in arresting caries was similar to atraumatic restorative treatment.13–15 When applied every six months, SDF arrests 91% of lesions within two years,14,16 and no significant benefit is found with excavation of caries prior to placement.17 Research shows that annual placement of SDF prevents more root caries in older adults than fluoride varnish or chlorhexidine varnish applied four times per year.10 In addition, more frequent placement appears to be safe and even more effective.14,18
Annual application was shown to provide high preventive effects in two studies of older adults, although another study did not support these results. A recent paper showed preventive rates of 90% after 30 months,19 while an earlier study showed a 71% preventive rate at three years.10 A third study, however, reported a preventive rate of 25% after two years.9 Additional research is needed in this area.
Repeated application, at least annually, appears to be critical to prevention and arrest. A dose-dependent improvement in effectiveness is seen with more frequent application15,18 and higher concentration.18,20 A case series with three applications over two weeks showed success in arresting caries, thereby eliminating the need for general anesthesia for an entire large community clinic.21 The pattern of a dose-dependent response suggests more frequent applications, depending on caries risk. Similar to a double-strength “loading dose” prescribed at the beginning of antibiotic regimens for difficult infections (e.g., diffuse cellulitis), with severe caries lesions, it is logical to “load” the lesions more frequently at the beginning of treatment. A recent clinical trial of SDF in preschoolers verified a more rapid response from a loading-dose approach.22
One of the greatest challenges that caries arrest poses is to continue monitoring lesions over years without jumping to operative treatment. The evidence supports patience. Studies show that with semiannual application, 44% of caries are arrested after six months, 61% after 12 months, 81% after 18 months, and by 24 months 91% of lesions are arrested.14,18 Because some lesions keep growing, however, monitoring progress is critical. It may be best to cover some lesions with a restorative material, such as glass ionomer cement, at a subsequent visit.
SIDEBAR: PROCEDURE BILLING CODE
The Code on Dental Procedures and Nomenclature Code Maintenance Commission has approved Code 1354 for “interim caries arresting medication application.” The code definition is for “conservative treatment of an active, nonsymptomatic carious lesion by topical application of a caries arresting or inhibiting medicament and without mechanical removal of sound tooth structure.” This is the Health Insurance Portability and Accountability Act standard code for billing purposes.
METHOD OF ACTION AND INDICATIONS FOR OLDER ADULTS
Upon application of SDF to a decayed surface, silver reacts with bacteria and dentin collagen23,24 to create a sclerotic silver-protein layer that is resistant to degradation.25 Hydroxyapatite and fluoroapatite form, along with metallic silver.26 The darkened, treated lesion hardens over a few weeks, while the lesion depth decreases.26,27 The silver inhibits bacterial enzymes that break down the organic dentin matrix.25,26,28 All caries-causing bacteria are susceptible to the effects of the silver ion.24,29,30 The silver stays latent in the lesion, so it is available to kill reinvading bacteria.31 Numerous clinicians have reported less plaque near treated teeth, and this has been reproduced in the laboratory.32,33 More silver and fluoride soaks into carious or demineralized than sound dentin; as a result, treated demineralized dentin is more resistant to caries bacteria.34
Among this patient population, the primary indications for topical treatment with SDF are:
- Disease control for lesions in high-caries-risk patients at the diagnostic visit, regardless of the restorative plan
- Difficult-to-treat caries lesions, such as furcations and crown margins
- Prevention for vulnerable surfaces — for example, gingival margins of compromised restorations, roots exposed from recession, and over-denture or partial denture abutments
- Patients with extreme caries risk (e.g., individuals experiencing xerostomia from cancer treatment or using hyposalivatory medications)
- Individuals who cannot cooperate because of Alzheimer’s disease or other forms of dementia, Parkinson’s disease, and other neuropsychiatric challenges
- Patients living in nursing homes and other residential facilities with limitations on mobility and/or ability to seek care
- Individuals without insurance benefits and/or living on fixed incomes
In these patients, SDF can be an effective first-stage treatment, and a component of long-term treatment (by continuing application twice per year, or more frequently, as indicated). This may be especially true with older adults who have physical or cognitive limitations that impede oral hygiene, or whose limited mobility poses challenges to oral health.
CLINICAL APPLICATION GUIDELINES
Recently, a team at the University of California, San Francisco School of Dentistry formalized best practices for SDF based on evidence and clinical experience. According to these clinical guidelines,13 when a clinician determines that an older adult would benefit from treatment, and without removing restorations or carious dentin, the lesion(s) are gently rinsed, isolated with cotton rolls, air dried, and a fraction of a drop of SDF is applied with a microsponge. Dryness of the surface and frequency of reapplication are thought to have the most significant impacts on efficacy. Whether in a distinct cavitated lesion or at the margin of a compromised restoration, the reaction between the material and lesion is protected from saliva for one to three minutes. There may be temporary staining of the gingiva, which resolves over a few days.
Anecdotally, there have been reports of clinicians achieving even better results by covering the treated lesion immediately with a varnish or petroleum jelly without a rinse. As a fluoride product, most states allow placement by dental auxiliaries, facilitating reapplication at recall or in situations in which clinicians are working independently in residential facilities.
Lesions change color within a week as they arrest, and eventually look similar to naturally arrested caries lesions. Upon application, patients will note a metallic taste, which resolves without intervention. Treated lesions harden to gentle probing over the course of a few weeks.
SAFETY CONSIDERATIONS
Cleared for marketing in the U.S. in 2014 and made available the next year, SDF’s regulatory parameters parallel that of fluoride varnish, as both are cleared for treating hypersensitivity, but are commonly applied in off-label use for caries management. After approval of SDF in Japan more than 45 years ago, no adverse events have been reported.35 Silver allergy — often confused with nickel allergy — is the only contraindication, but it is rare. Adults can tolerate considerable silver consumption chronically. With reasonable caution to use sparing amounts, this acute fluoride exposure does not present a safety concern.36,37
The relatively high concentration of ammonia appears to be the primary safety consideration. Using microliter volumes that are absorbed mainly into lesions, the cautious clinician will do no harm. If there is a breakdown of the protective barrier formed by gingiva or mucosa, the area should be protected with a thin layer of petroleum jelly. Universal precautions should be followed when using SDF. Topical application to the oral mucosa or skin can leave a temporary tattoo that will disappear without treatment in approximately two weeks.
In addition to darkening caries lesions, SDF can stain countertops and floors, although ammonia-based commercial cleaning agents or simply salt with a little water have been seen to remove stains not cleared by standard clinical disinfectants.
CONCLUSION
Newly available to U.S. clinicians, SDF is an evidence-based technology that offers an effective approach to caring for older adults. Indications include treating caries and recurrent decay, particularly in hard-to-access areas, such as furcations. Its indications as a preventive agent are based on high caries risk, and risk of caries due to the complexities of other therapies.
Cognitive disabilities (such as Alzheimer’s disease), physical disabilities (such as Parkinson’s disease or multiple sclerosis), and situational challenges (such as a lack of mobility or residing in long-term care facilities) often limit older adults’ access to traditional dentistry. The use of SDF provides an alternative treatment modality that is consistent with the principles of caries balance. In addition, it does not interfere with other professional or self-care activities needed to restore and maintain caries control. Adding SDF to the armamentarium makes caries arrest practically feasible and enables extension of care to vulnerable populations.
Acknowledgements: The author would like to thank Susan Hyde, DDS, MPH, PhD, director of the Multidisciplinary Geriatrics Fellowship and chair of Oral Epidemiology and Dental Public Health at the University of California, San Francisco (UCSF), Nathan G. Kaufman, DDS, and Steve Duffin, DDS, for their contributions to this manuscript. He also thanks John D.B. Featherstone, PhD, dean of the UCSF School of Dentistry, for his guidance and support. The author was supported by the National Institute of Dental and Craniofacial Research Comprehensive Oral Health Training Program: NIH T32-DE007306.
References
- Walls AWG, Meurman JH. Approaches to caries prevention and therapy in the elderly. Adv Dent Res. 2012;24:36–40.
- Nasseh K, Vujicic M. American Dental Association Health Policy Resources Center Research Brief. Dental Care Utilization Continues to Decline Among Working- Age adults, Increases Among the Elderly, Stable Among Children. Available at: ada.org/~/media/ADA/Science%20and%2 0Research/Files/HPRCBrief_1013_2.pdf. Accessed July 18, 2016.
- Griffin SO, Jones JA, Brunson D, Griffin PM, Bailey WD. Burden of oral disease among older adults and implications for public health priorities. Am J Public Health. 2012;102:411–418.
- Griffin SO, Griffin PM, Swann JL, Zlobin N. Estimating rates of new root caries in older adults. J Dent Res. 2004;83:634–638.
- Gregory D, Hyde S. Root caries in older adults. J Calif Dent Assoc. 2015;43:439–445.
- McComb D, Erickson RL, Maxymiw WG, Wood RE. A clinical comparison of glass ionomer, resin-modified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Oper Dent. 2002;27:430–437.
- Mei ML, Chu CH, Lo ECM, Samaranayake LP. Fluoride and silver concentrations of silver diammine fluoride solutions for dental use. Int J Paediatr Dent. 2013;23:279–285.
- Rosenblatt A, Stamford TCM, Niederman R. Silver diamine fluoride: A caries “silver-fluoride bullet.” J Dent Res. 2009;88:116–125.
- Zhang W, McGrath C, Lo ECM, Li JY. Silver diamine fluoride and education to prevent and arrest root caries among community-dwelling elders. Caries Res. 2013;47:284–290.
- Tan HP, Lo ECM, Dyson JE, Luo Y, Corbet EF. A randomized trial on root caries prevention in elders. J Dent Res. 2010;89:1086–1090.
- Chu CH, Lee AH-C, Zheng L, Mei ML, Chan GC-F. Arresting rampant dental caries with silver diamine fluoride in a young teenager suffering from chronic oral graft versus host disease post-bone marrow transplantation: a case report. BMC Res Notes. 2014;7:3.
- Milgrom P. Management of patients with active caries. J Calif Dent Assoc. 2014;42:449–453.
- Horst JA, Ellenikiotis H, Milgrom P. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016;44:16–28.
- Zhi QH, Lo ECM, Lin HC. Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40:962–967.
- Santos VE Jr, Vasconcelos Filho A, Targino AG, et al. A new “silver-bullet” to treat caries in children — nano silver fluoride: a randomised clinical trial. J Dent. 2014;42:945–951.
- Llodra JC, Rodriguez A, Ferrer B, Menardia V, Ramos T, Morato M. Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84:721–724.
- Chu CH, Lo ECM, Lin HC. Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese pre-school children. J Dent Res. 2002;81:767–770.
- Fung HTM, Duangthip D, Wong MCM, Lo ECM, Chu CH. Arresting dentine caries with different concentration and periodicity of silver diamine fluoride. JDR Clinical & Translational Research. 2016;1(2):143–152.
- Li R, Lo ECM, Liu BY, Wong MCM, Chu CH. Randomized clinical trial on arresting dental root caries through silver diammine fluoride applications in community-dwelling elders. J Dent. 2016;51:15–20.
- Yee R, Holmgren C, Mulder J, Lama D, Walker D, van Palenstein Helderman W. Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 2009;88:644–647.
- Duffin S. Back to the future: the medical management of caries introduction. J Calif Dent Assoc. 2012;40:852–858.
- Duangthip D, Chu CH, Lo ECM. A randomized clinical trial on arresting dentine caries in preschool children by topical fluorides —18 month results. J Dent. 2016;44:57–63.
- Klasen HJ. A historical review of the use of silver in the treatment of burns. II. Renewed interest for silver. Burns. 2000;26:131–138.
- Youravong N, Carlen A, Teanpaisan R, Dahlén G. Metal-ion susceptibility of oral bacterial species. Lett Appl Microbiol. 2011;53:324–328.
- Mei ML, Li QL, Chu CH, Yiu CKY, Lo ECM. The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater. 2012;28:903–908.
- Mei ML, Ito L, Cao Y, Li QL, Lo ECM, Chu CH. Inhibitory effect of silver diamine fluoride on dentine demineralisation and collagen degradation. J Dent. 2013;41:809–817.
- Mei ML, Ito L, Cao Y, Lo ECM, Li QL, Chu CH. An ex vivo study of arrested primary teeth caries with silver diamine fluoride therapy. J Dent. 2014;42:395–402.
- Mei ML, Ito L, Cao Y, Li QL, Chu CH, Lo ECM. The inhibitory effects of silver diamine fluorides on cysteine cathepsins. J Dent. 2014;42:329–335.
- Thibodeau EA, Handelman SL, Marquis RE. Inhibition and killing of oral bacteria by silver ions generated with low intensity direct current. J Dent Res. 1978;57:922–926.
- Thurman RB, Gerba CP. The molecular mechanisms of copper and silver ion disinfection of bacteria and viruses. CRC Crit Rev Environ Control. 1989;18:295–315.
- Englander HR, James VE, Massler M. Histologic effects of silver nitrate of human dentin and pulp. J Am Dent Assoc. 1958;57:621–630.
- Knight GM, McIntyre JM, Craig GG, Mulyani, Zilm PS, Gully NJ. Inability to form a biofilm of Streptococcus mutans on silver fluoride- and potassium iodide-treated demineralized dentin. Quintessence Int. 2009;40:155–161.
- Knight GM, McIntyre JM, Craig GG, Mulyani, Zilm PS, Gully NJ. An in vitro model to measure the effect of a silver fluoride and potassium iodide treatment on the permeability of demineralized dentine to Streptococcus mutans. Aust Dent J. 2005;50:242–245.
- Knight GM, McIntyre JM, Craig GG, Mulyani, Zilm PS, Gully NJ. Differences between normal and demineralized dentine pretreated with silver fluoride and potassium iodide after an in vitro challenge by Streptococcus mutans. Aust Dent J. 2007;52:16–21.
- Chu CH, Lo ECM. Promoting caries arrest in children with silver diamine fluoride: a review. Oral Health Prev Dent. 2008;6:315–321.
- Vasquez E, Zegarra G, Chirinos E, et al. Short term serum pharmacokinetics of diammine silver fluoride after oral application. BMC Oral Health. 2012;12:60.
- Milgrom P, Taves DM, Kim AS, Watson GE, Horst JA. Pharmacokinetics of fluoride in toddlers after application of 5% sodium fluoride dental varnish. Pediatrics. 2014;134:e870–e874.
From Decisions in Dentistry. August 2016;2(08):30–33.





[…] And lastly, another link to a dental publication about using SDF in older populations: […]
[…] for use in the United States. 2 Horst JA. Silver diamine fluoride use in older adults. Decisions in Dentistry. 2016;2(08):30–33. 3Mei ML, Chu CH, Lo EC, Samaranayake LP. Fluoride and silver concentrations of […]