
Retention of the Natural Dentition and Replacement of Missing Teeth
Biological and technical advances — combined with appropriate treatment planning and care — are helping patients achieve long-term retention of their natural dentition.
Preservation of the natural dentition is the primary goal of dentistry. Published surveys indicate that patients value teeth and, whenever possible, express a desire to save their natural dentition in favor of extraction.1,2 Significant technological and biological improvements in all disciplines of dentistry have made long-term retention of natural teeth more attainable. Patients entrust oral health professionals to make appropriate recommendations regarding the maintenance and restoration of their oral health and function. As a provider, it is essential to employ an evidence-based, interdisciplinary approach that addresses the interests of the patient when determining the best possible course of treatment.
In July 2014, the American Association of Endodontists (AAE), in collaboration with the American College of Prosthodontists and the American Academy of Periodontology, hosted a joint symposium, “Teeth for a Lifetime: Interdisciplinary Evidence for Clinical Success.” Approximately 375 general dentists and specialists assembled in Chicago to focus on preserving the natural dentition. The educational program included evidence-based presentations on advanced regenerative techniques, improvements in technology, minimally invasive restorative methods, and best practices for interdisciplinary treatment planning. When developing treatment plans, Alan H. Gluskin, DDS, chair of the 2014 Joint Symposium Planning Committee, concluded that the current evidence directs clinicians to consider saving the natural dentition as the first option.
Dental implants are one of the most significant advances in contemporary dentistry. This innovation has had profound effects on endodontic, periodontic and prosthodontic treatment planning for the rehabilitation of edentulous spaces, and for teeth with an unfavorable prognosis.3 Implant-supported restorations minimize unnecessary preparation of intact abutment teeth, and allow fixed prosthodontic replacement when suitable abutments are absent. With appropriate usage and case selection, implants are a viable option for the replacement of missing teeth.4,5
There has been a growing trend of replacing diseased teeth with implants. Often, an inadequate or inappropriate indication for tooth extraction has resulted in the removal of teeth that may have been salvageable.6 Teeth compromised by pulpal or periodontal disease should not be extracted without thoroughly evaluating restorability and potential retention therapies.7
A systematic review published in the Journal of the American Dental Association highlights a key question: “Is the long-term survival rate of dental implants comparable to that of periodontally compromised natural teeth that are adequately treated and maintained?”8 Nineteen studies with a follow-up period of at least 15 years were included in the analysis. The results show that implant survival rates do not exceed those of compromised, but adequately treated and maintained, teeth. These findings support other studies comparing long-term survival of implants and natural teeth,9,10 and serve as an important message: Periodontally compromised teeth can be retained with quality treatment and appropriate maintenance. Therefore, it may be advisable to postpone implant consideration for the periodontitis-susceptible patient to fully utilize and extend the capacity of the natural dentition.11
TREATMENT PLANNING OPTIONS
A key focus of the joint symposium involved treatment planning decisions regarding endodontic treatment and implant therapy. Should a tooth with pulpal disease be retained with root canal treatment and restoration, or be extracted and replaced with an implant-supported restoration? This assessment involves a challenging and complex decision-making process that must be customized to suit the patient’s needs and desires.12–14 The topic has received considerable attention in the literature and media, as well as in continuing education courses.

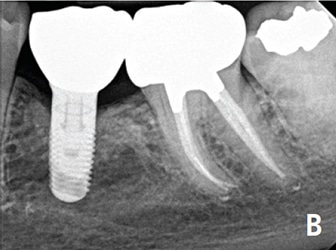
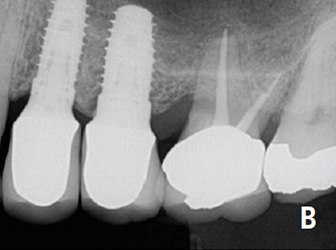
Endodontic treatment and implant therapy should not be viewed as competing alternatives, but, rather, as complementary options for the appropriate patient situation (Figures 1A and 1B). Root canal treatment is indicated for restorable, periodontally sound teeth with pulpal and/or apical pathosis. Endodontic treatment for teeth with nonrestorable crowns or severe periodontal conditions is contraindicated, and other options, such as implant placement, should be considered.15 When making treatment decisions, the clinician should weigh multiple factors, including outcome assessment, local and systemic case-specific issues, cost, the patient’s desires and needs, esthetics and ethical considerations.16
SUCCESS AND SURVIVAL
Treatment outcomes play a key role in the assessment of various treatment options. Patients often ask whether a procedure is going to be successful. This can be challenging to answer due to the variety of reported outcomes in the literature.17 Differences in the methodology and criteria used to evaluate the outcomes for root canal treatment and implant prosthetics make comparisons between success rates difficult, if not impossible.18 Endodontic studies have historically used “success” and “failure” as outcome measures, and have focused on a strict combination of radiographic and clinical criteria.19 In contrast, the implant literature has primarily reported “survival”20,21 (i.e., the implant is either present or absent). Therefore, implant studies that solely evaluate survival will likely publish higher success rates than endodontic studies that rely on biologic healing and factors related to the entire restored tooth. To establish more valid and less biased comparisons, the same outcome measures should be used. A more patient-centered measure, for example, is to compare the outcome of survival, which is considered to be an asymptomatic tooth/implant that is present and functioning.22,23
Multiple large-scale studies of millions of teeth have used survival to assess outcomes following root canal treatment. An investigation using an insurance database of more than 1.4 million root canal-treated teeth demonstrated that 97% were retained within an eight-year follow-up period.24 Other studies show similar survival rates.25,26 An epidemiological approach allows for the assessment of tooth retention from a large sample of patients experiencing actual care in private practice. Systematic reviews27 and controlled studies from academic settings complement the previous findings. Two prospective trials reported 95% survival rates at four years,28 and four to six years,29 respectively, for teeth following initial root canal therapy.
NONSURGICAL ROOT CANAL TREATMENT AND RESTORATION
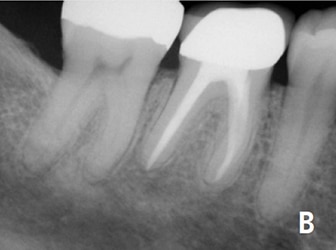
The majority of endodontic treatment is performed by general dentists — and with a high degree of success.26 For complex cases, referral to an endodontist may result in more favorable outcomes30 and positive patient experiences.31 Interdisciplinary care is important for the management of endodontically treated teeth. The restorative dentist plays a significant role in the outcome by providing an appropriate and timely restoration.32 Root canal treatment is not complete until the tooth is coronally sealed and restored to function. Multiple studies have confirmed that a definitive restoration has a significant impact on tooth survival.24,25,27,28,33 Therefore, the likelihood of a favorable outcome increases with both skillful endodontic care and prompt restorative treatment (Figures 2A and 2B).34

Advances in technology aid clinicians in attaining high levels of tooth retention. The dental operating microscope, nickel-titanium instruments, apex locators, enhanced irrigation protocols, and dentin preservation strategies are examples of improvements that allow operators to predictably manage a greater range of treatment options. Additionally, cone beam computed tomography facilitates more accurate diagnosis and improved decision-making for the management of endodontic conditions.35,36

ENDODONTIC TREATMENT AND SINGLE-TOOTH IMPLANTS
Large-scale systematic reviews have addressed the relative survival rates of endodontically treated teeth and single-tooth implants. The Academy of Osseointegration conducted a meta-analysis using 13 studies of restored endodontically treated teeth (involving approximately 23,000 teeth), and 57 studies of single-tooth implants (involving 12,000 implants). The data demonstrated no difference between the two groups during any of the observation periods.37 Another systematic review compared the outcomes of endodontically treated teeth with those of a single-tooth implant-restored crown, fixed partial denture, or no treatment after extraction. At 97%, the long-term survival rate was essentially the same for implant and endodontic therapies. Both options were superior to extraction and replacement of the missing tooth with a fixed partial denture.38
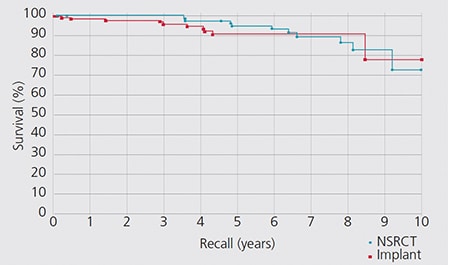
Retrospective studies also have compared the outcomes for these two treatment options. A study by the University of Minnesota compared the outcomes of 196 restored endodontically treated teeth with 196 matched single-tooth implants.39 Both groups had 94% survival rates. The survival curves for these two groups are provided in Figure 3. An investigation by the University of Alabama provided similar results.40
Based upon similar survival rates, the decision to treat a compromised tooth endodontically or replace it with an implant must be based on factors other than treatment outcome.37,41 Several factors influence the decision-making process.42–44 The following lists provide an overview of case-specific factors that should be considered when making this treatment decision:
Systemic Factors
- The list of potential risk factors for peri-implantitis or implant failure is extensive, and includes systemic disease, genetic traits, chronic drug or alcohol consumption, smoking, periodontal disease, radiation therapy, diabetes, osteoporosis, dental plaque and poor oral hygiene.45
- There are few medical conditions that directly affect endodontic treatment outcomes. Risk factors that may be associated with decreased survival of endodontically treated teeth include smoking,46 diabetes,28,46 systemic steroid therapy28 and hypertension.47
- Patients taking antiangiogenic or antiresorptive (e.g., bisphosphonate) medications may have an increased risk for developing medication-related osteonecrosis of the jaw. This may affect treatment planning for both implant and endodontic therapy.
- It is generally recommended to wait for the completion of dental and skeletal growth prior to implant placement.48
Local Factors
- Accurate diagnosis.
- Restorability assessment: removal of caries/restorations; adequate ferrule.
- Strategic nature of the tooth as it fits into the comprehensive restorative plan.
- Caries risk and oral hygiene.
- Periodontal assessment: tissue biotype, adequate biologic width.
- Presence of crack(s), root fracture(s) and/or resorption.
- Occlusion and parafunction.
- Teeth with less than two proximal contacts, and those serving as fixed partial denture abutments may have lower survival rates.27
- Need for adjunctive treatment (such as crown lengthening, orthodontic extrusion, sinus lift or bone graft) that may impact financial cost and time to function.
- Quantity and quality of bone.
- Proximity to anatomical structures (e.g., the maxillary sinus and/or inferior alveolar nerve).
- Challenging implant esthetics in the anterior region.49
In addition to systemic and local factors, it is critical to consider the patient’s concerns during treatment planning. Common patient-centered concerns include cost, treatment duration, satisfaction with treatment, and the potential for adverse outcomes.
When weighing treatment options, financial considerations can influence patient decisions. The availability of dental insurance may also impact choices.50 Endodontic treatment and restoration offer considerable economic advantages to the patient.51–53 A benefit of root canal treatment is the short time frame required to completely restore function and esthetics. In a study of approximately 400 subjects, restored single-tooth implants showed a longer average and median time to function than similarly restored, endodontically treated teeth. Additionally, the implant group had a higher incidence of posttreatment complications that required subsequent intervention.39 The resulting increased postoperative care can impact patients in terms of additional visits, lost wages and unforeseen costs.
Clinicians should consider the patient’s preferences, which are often related to function, comfort and esthetics. Tooth loss is associated with an impaired quality of life,54 and, as noted, surveyed patients express a desire to save their natural dentition whenever possible.2 Large-scale surveys of postendodontic patients have demonstrated that endodontic treatment not only helps preserve the natural tooth, it also improves patients’ quality of life.55 More than 97% of patients report being satisfied with their endodontic treatment.31 If an implant is used to restore an edentulous space, a similarly high percentage report a positive experience with implant therapy.56 Furthermore, comparative studies demonstrate that patients indicate a high degree of satisfaction with the overall experience following either procedure.2,15
Despite high survival rates, endodontically treated teeth and implants are both susceptible to complications. Nonrestorable caries, prosthetic failures, periodontal disease, crown/root fractures and specific endodontic factors are examples of complications following root canal therapy.57 Complications associated with implants and related prostheses include surgical, implant loss, bone loss, peri-implant soft-tissue, mechanical and esthetic/phonetic.58 A retrospective study that directly compared the rates of additional interventions related to complications found that implant patients had a substantially higher need for subsequent intervention and maintenance visits than endodontically treated teeth.40 However, a more recent prospective study suggests that patients from both groups have minimal complications at the 12-month follow-up.15
ENDODONTIC RETREATMENT OPTIONS
The consequences of failure and subsequent treatment differ between endodontics and implants. Endodontic failure can usually be addressed successfully by retreatment, microsurgery, or by extraction and potential implant placement. Intervention after implant failure may vary from minimal restorative repairs to multiple corrective surgeries and/or the use of a different prosthesis.59
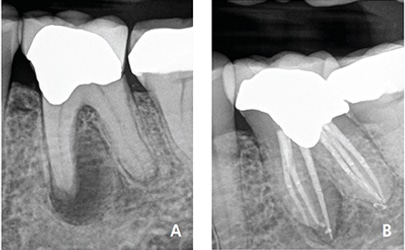
Nonsurgical retreatment, or revision, is often the first choice to address posttreatment apical periodontitis,60,61 provided the tooth is suitable for further restoration and the restoration will have a good long-term prognosis (Figures 4A and 4B).62 Current best evidence indicates that the survival of nonsurgical retreatment is similar to that of primary treatment, and that the two treatments share similar prognostic factors.63 Two studies specifically evaluated survival following retreatment. An epidemiological study using an insurance database of 4744 retreated teeth reported an 89% survival rate at five years,64 while a prospective trial of 858 retreated teeth noted 95% survival at four years.28

Modern techniques and rationale contribute to excellent potential outcomes for retreatment. An important factor when considering retreatment is the ability to identify and address the etiology of posttreatment disease.63 Primary sources of nonhealing are persistent intracanal microorganisms, or ingress of microorganisms following treatment. If the etiology of the problem is deemed correctable via an orthograde approach, retreatment is often the first choice. If not, a surgical approach may be the more predictable option.65
Contemporary endodontic microsurgery has undergone significant technological and procedural advances.66,67 Recent studies suggest that microsurgical techniques using biocompatible root-end filling materials provide significant improvements over traditional methods. A meta-analysis showed contemporary microsurgical techniques offer significantly improved outcomes (94%), compared to older techniques and instruments (59%).68 A systematic review investigating current microsurgery found survival rates of 94% at two to four years, and 88% at four to six years, indicating that teeth treated with endodontic microsurgery tended to be lost at low rates over the time studied.69 Microsurgery, with appropriate case selection, is a predictable procedure for teeth that may have been candidates for extraction in the past.
ETHICS AND INTERDISCIPLINARY CONSULTATION
Clinicians are ethically bound to inform patients of all reasonable treatment options, explain the risks and benefits involved, and obtain informed consent before initiating therapy. This information should be conveyed in an impartial manner.1 Patients value participation in the decision-making process and should be encouraged to exercise autonomy by communicating their preferences.70 Clinical decisions regarding either endodontic treatment or tooth extraction with implant therapy must always be made in the best interest of the patient, and using the best and most current evidence.
Should it be necessary, experts may need to be called upon to assist the clinician in rendering the highest quality of care (Figures 5A and 5B). The standard of care must be applied equally to all clinicians — generalists and specialists alike. The AAE’s Endodontic Case Difficulty Assessment Form and Guidelines provide valuable information to aid in case selection and determining whether to treat or refer. Patients deserve the best possible outcome in every case, and interdisciplinary communication and collaboration during treatment planning and care maximizes this likelihood.
Specialists and restorative dentists should be viewed as partners on the treatment planning team. Endodontists are uniquely positioned to evaluate the restorability and prognostic longevity of teeth and recommend whether to attempt tooth preservation or consider extraction and replacement with an implant.71 Likewise, the endodontist should be well-versed in implant treatment planning to assist patients and referring colleagues in making an informed choice regarding replacement options.72,73
If a tooth has a questionable prognosis, the endodontist becomes an indispensable part of the treatment planning team. Endodontists have experience with various treatment options that have potential to preserve the natural dentition. Consultation regarding a questionable tooth is often in the patient’s best interest prior to considering extraction. If the prognosis of a restorable tooth is categorized as questionable or unfavorable in multiple areas of evaluation, extraction should be considered — but only after appropriate consultation with all relevant specialists. Only then is the decision to extract an informed choice. Extraction is an irreversible treatment, but, if necessary, dental implants provide an excellent option to replace missing teeth (Figures 6A and 6B).

CONCLUSION
Patients are living longer, which makes preservation of the natural dentition more important than ever. Helping patients maintain their teeth for a lifetime is the fundamental goal of dentistry. A wide range of endodontic therapies can help support tooth retention and patient satisfaction. Large-scale studies provide strong evidence that the restored, endodontically treated tooth offers a highly predictable, long-term approach to preserving “nature’s implant” — a tooth with an intact periodontal ligament. Thus, excellent endodontic treatment, followed by an immediate restoration of equal quality, promises to ensure patients years of service and function while maintaining esthetics.
The results of multiple studies indicate that high survival rates for natural teeth are similar to those reported for the restored single-tooth implant. Therefore, clinicians must consider additional factors when making treatment planning decisions — all of which must be in the best interest of the patient. As noted, endodontic treatment and implant therapy should not be viewed as competing alternatives, but, rather, as complementary treatment options for the appropriate patient situation.
KEY TAKEAWAYS
- Significant technological and biological improvements in all disciplines of dentistry have made long-term retention of natural teeth more attainable.
- Teeth compromised by pulpal or periodontal disease should not be extracted without thoroughly evaluating restorability and potential retention therapies.7
- When making treatment decisions, the clinician should consider outcome assessment, local and systemic case specific issues, cost, the patient’s desires, esthetics and
ethical considerations.16 - Endodontic treatment and implant therapy should not be viewed as competing alternatives, but, rather, as complementary options for the appropriate patient situation.
- Interdisciplinary care is important in the management of endodontically treated teeth.
- The majority of endodontic treatment is performed by general dentists, and with a high degree of success26 — but, for complex cases, referral to an endodontist may
result in more favorable outcomes.30
A version of this article originally appeared in ENDODONTICS: Colleagues for Excellence, Spring 2015. Reused with permission from the American Association of Endodontists, ©2015. The AAE clinical newsletter is available at aae.org/colleagues.
REFERENCES
- Azarpazhooh A, Dao T, Figueiredo R, Krahn M, Friedman S. A survey of patients’ preferences for the treatment of teeth with apical periodontitis. J Endod. 2013;39:1534–1541.
- Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N. Quality of life of endodontically treated versus implant treated patients: a university-based qualitative research study. J Endod. 2011;37:903–909.
- Baba NZ, Goodacre CJ, Kattadiyil MT. Tooth retention through root canal treatment or tooth extraction and implant placement: a prosthodontic perspective. Quintessence Int. 2014;45:405–416.
- Moraschini V, Poubel LA, Ferreira VF, Barboza Edos S. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg. 2015;44:377–388.
- Pjetursson BE, Asgeirsson AG, Zwahlen M, Sailer I. Improvements in implant dentistry over the last decade: comparison of survival and complication rates in older and newer publications. Int J Oral Maxillofac Implants. 2014;29(Suppl):308–324.
- Avila G, Galindo-Moreno P, Soehren S, Misch CE, Morelli T, Wang HL. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80:476–491.
- Lindhe J, Pacey L. There is an overuse of implants in the world and an underuse of teeth as targets for treatment. Br Dent J. 2014;217:396–397.
- Levin L, Halperin-Sternfeld M. Tooth preservation or implant placement: a systematic review of long-term tooth and implant survival rates. J Am Dent Assoc. 2013;144:1119–1133.
- Tomasi C, Wennström JL, Berglundh T. Longevity of teeth and implants – a systematic review. J Oral Rehabil. 2008;35(Suppl 1):23–32.
- Holm-Pedersen P, Lang NP, Müller F. What are longevities of teeth and oral implants? J Clin Oral Implant Res. 2007;18(Suppl 3):15–19.
- Lundgren D, Rylander H, Laurell L. To save or extract, that is the question. Natural teeth or dental implants in periodontitis-susceptible patients: clinical decision-making and treatment strategies exemplified with patient case presentations. Periodontol 2000. 2008;47:27–50.
- Pradeep K, Rajesh H, Rao PK, Hedge SK, Shetty HK. Implant or root canal treatment: clinical guidelines and decision making. J Dent Implant. 2013;3:67–72.
- Zitzmann NU, Krastl G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J. 2009;42:757–774.
- John V, Chen S, Parashos P. Implant or the natural tooth–a contemporary treatment planning dilemma? Aust Dent J. 2007;52(1 Suppl):S138–150.
- Torabinejad M, Salha W, Lozada JL, Hung YL, Garbacea A. Degree of patient pain, complications, and satisfaction after root canal treatment or a single implant: a preliminary prospective investigation. J Endod. 2014;40:1940–1945.
- American Association of Endodontists. Treatment Options for the Compromised Tooth: A Decision Guide. Available at: aae.org/uploadedfiles/clinical_resources/treatment_planning/2014treatmentoptionsguidefinalweb.pdf. Accessed October 10, 2017.
- Stockhausen R, Aseltine R Jr, Matthews JG, Kaufman B. The perceived prognosis of endodontic treatment and implant therapy among dental practitioners. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:42–47.
- Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res. 2014;93:19–26.
- Strindberg LZ. The dependence of the results of pulp therapy on certain factors. An analytic study based on radiographic and clinical follow-up examinations. Acta Odontol Scand. 1956;14(Suppl 21):1–175.
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO. Success criteria in implant dentistry: a systematic review. J Dent Res. 2012;91:242–248.
- Bhatavadekar N. Helping the clinician make evidence-based implant selections. A systematic review and qualitative analysis of dental implant studies over a 20 year period. Int Dent J. 2010;60:359–369.
- American Association of Endodontists. Implants. AAE Position Statement 2007. Available at: aae.org/uploadedfiles/clinical_resources/guidelines_and_position_statements/implantsstatement.pdf. Accessed October 10,2017.
- Friedman S, Mor C. The success of endodontic therapy-healing and functionality. J Calif Dent Assoc. 2004;32:493–503.
- Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846–850.
- Chen SC, Chueh LH, Hsiao CK, Tsai MY, Ho SC, Chiang CP. An epidemiologic study of tooth retention after nonsurgical endodontic treatment in a large population in Taiwan. J Endod. 2007;33:226–229.
- Lazarski MP, Walker WA 3rd, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J Endod. 2001;27:791–796.
- Ng YL, Mann V, Gulabivala K. Tooth survival following non-surgical root canal treatment: a systematic review of the literature. Int Endod J. 2010;43:171–189.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44:610–625.
- de Chevigny C, Dao TT, Basrani BR, et al. Treatment outcome in endodontics: the Toronto study—phase 4: initial treatment. J Endod. 2008;34:258–63.
- Alley BS, Kitchens GG, Alley LW, Eleazer PD. A comparison of survival of teeth following endodontic treatment performed by general dentists or by specialists. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:115–118.
- Dugas NN, Lawrence HP, Teplitsky P, Friedman S. Quality of life and satisfaction outcomes of endodontic treatment. J Endod. 2002;28:819–827.
- Baba NZ, Goodacre CJ. Restoration of endodontically treated teeth: contemporary concepts and future perspectives. Endod Topics. 2014;31:68–83.
- Aquilino SA, Caplan DJ. Relationship between crown placement and the survival of endodontically treated teeth. J Prosthet Dent 2002;87:256–263.
- Gillen BM, Looney SW, Gu LS, et al. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod. 2011;37:895–902.
- Patel S, Durack C, Abella F, et al. Cone beam computed tomography in endodontics–a review. Int Endod J. 2015;48:3–15.
- Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014;40:910–916.
- Iqbal MK, Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants. 2007;22(Suppl):96–116.
- Torabinejad M, Anderson P, Bader J, et al. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98:285-311.
- Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR. Retrospective cross-sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod. 2006;32:822–827.
- Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod. 2008;34:1302–1305.
- Iqbal MK, Kim S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod. 2008;34:519–529.
- Torabinejad M, Goodacre CJ. Endodontic or dental implant therapy: the factors affecting treatment planning. J Am Dent Assoc. 2006;137:973–977.
- Doyle SL, Hodges JS, Pesun IJ, Baisden MK, Bowles WR. Factors affecting outcomes for single-tooth implants and endodontic restorations. J Endod. 2007;33:399–402.
- Morris MF, Kirkpatrick TC, Rutledge RE, Schindler WG. Comparison of nonsurgical root canal treatment and single-tooth implants. J Endod. 2009;35:1325–1330.
- Dawson DR 3rd, Jasper S. Key systemic and environmental risk factors for implant failure. Dent Clin North Am. 2015;59:25–39.
- Bowles WR, Drum M, Eleazer PD. Endodontic and implant algorithms. Dent Clin North Am. 2010;54:401-413.
- Wang CH, Chueh LH, Chen SC, Feng YC, Hsiao CK, Chiang CP. Impact of diabetes mellitus, hypertension, and coronary artery disease on tooth extraction after nonsurgical endodontic treatment. J Endod. 2011;37:1–5.
- Mankani N, Chowdhary R, Patil BA, Nagaraj E, Madalli P. Osseointegrated dental implants in growing children: a literature review. J Oral Implantol. 2014;40:627–631.
- Fuentealba R, Jofré J. Esthetic failure in implant dentistry. Dent Clin North Am. 2015;59:227–246.
- Reese R, Aminoshariae A, Montagnese T, Mickerl A. Influence of demographics on patients’ receipt of endodontic therapy or implant placement. J Endod. 2015;41:470–472.
- Christensen GJ. Implant therapy versus endodontic therapy. J Am Dent Assoc. 2006;137:1440–1443.
- Pennington MW, Vernazza CR, Shackley P, Armstrong NT, Whitworth JM, Steele JG. Evaluation of the cost-effectiveness of root canal treatment using conventional approaches versus replacement with an implant. Int Endod J. 2009;42:874–883.
- Kim SG, Solomon C. Cost-effectiveness of endodontic molar retreatment compared with fixed partial dentures and single-tooth implant alternatives. J Endod. 2011;37:321–325.
- Gerritsen AE, Allen PF, Witter DJ, Bronkhorst EM, Creugers NH. Tooth loss and oral health-related quality of life: a systematic review and meta-analysis. Health Qual Life Outcomes. 2010;8:126.
- Liu P, McGrath C, Cheung GS. Improvement in oral health-related quality of life after endodontic treatment: a prospective longitudinal study. J Endod. 2014;40:805–810.
- Pjetursson BE, Karoussis I, Bürgin W, Brägger U, Lang NP. Patients’ satisfaction following implant therapy. A 10-year prospective cohort study. Clin Oral Implants Res. 2005;16:185–193.
- Zitzmann NU, Krastl G, Hecker H, Walter C, Waltimo T, Weiger R. Strategic considerations in treatment planning: deciding when to treat, extract, or replace a questionable tooth. J Prosthet Dent. 2010;104:80–91.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90:121–132.
- White SN, Miklus VG, Potter KS, Cho J, Ngan AY. Endodontics and implants, a catalog of therapeutic contrasts. J Evid Based Dent Pract. 2006;6:101–109.
- Friedman S. Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). Endod Topics. 2002;1:54–78.
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009;35:930–937.
- Abbott PV. Diagnosis and management planning for root-filled teeth with persisting or new apical pathosis. Endod Topics. 2011;19:1–21.
- Ng YL, Gulabivala K. Outcome of non-surgical re-treatment. Endod Topics. 2011;18:3–30.
- Salehrabi R, Rotstein I. Epidemiologic evaluation of the outcomes of orthograde endodontic retreatment. J Endod. 2010;36:790–792.
- Gorni FG, Gagliani MM. The outcome of endodontic retreatment: a 2-yr follow-up. J Endod. 2004;30:1–4.
- Niemczyk SP. Essentials of endodontic microsurgery. Dent Clin North Am. 2010;54:375–399.
- Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32:601–623.
- Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature–part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010;36:1757–1765.
- Torabinejad M, Landaez M, Milan M, et al. Tooth retention through endodontic microsurgery or tooth replacement using single implants: a systematic review of treatment outcomes. J Endod. 2015;41:1–10.
- Azarpazhooh A, Dao T, Ungar WJ, et al. Clinical decision making for a tooth with apical periodontitis: the patients’ preferred level of participation. J Endod. 2014;40:784–789.
- Silvestrin T. The role of implant dentistry in the specialty of endodontics. Endod Topics. 2014;30:66–74.
- Cohn SA. Treatment choices for negative outcomes with non-surgical root canal treatment: non-surgical retreatment vs. surgical retreatment vs. implants. Endod Topics. 2005;11:4–24.
- Torabinejad M, Sabeti M, Goodacre C. Principles and Practice of Single Implant and Restorations. St. Louis, Mo: Saunders; 2014.
The author has no commercial conflicts of interest to disclose.
Featured image by FIKMIK/ISTOCK/GETTY IMAGES PLUS
From Decisions in Dentistry. November 2017;3(11):12,14,16–17.



[…] Through his research, Chai aims to find ways to regenerate a molar root and place a crown on it. “It would be the best of both worlds,” he says, “a natural integration of the root with the jawbone with the periodontal ligament in place, and a reduction in the amount of time we need by using just a crown to restore function.” Read more about “Retention of the Natural Dentition and Replacement of Missing Teeth” […]