
Pathologic Tooth Migration and Diastemata
Tooth drifting in adults may be a warning sign of advanced periodontitis — and severe cases may require a multidisciplinary approach.
Diastemata are common findings in the daily practice of dentistry. Some develop during the mixed dentition period, but most of these diastemata close after the eruption of the permanent canines. The formation of diastemata in adult patients, however, may be a sign of oral disease, such as advanced periodontitis.

Diastemata are a normal sequela of jaw growth and development. The most common diastemata occur between the maxillary central incisors. The prevalence of diastemata in young children is quite high, ranging from 43% to 97%.1–3 The prevalence decreases by the time children reach 11 and is gradually eliminated by age 15 in most children. Diastemata result from discrepancies between the growth of the jaws and the sizes of the erupted teeth. The transition from the primary to the permanent dentition is characterized by an enlargement of the jaws with the creation of additional space to accommodate permanent teeth that significantly differ in size and number from the deciduous dentition. Thus, diastemata between the maxillary central incisors is commonplace during the mixed dentition years. In most cases, such diastemata resolve after eruption of the permanent maxillary lateral incisors and canines (Figure 1 to Figure 3).4

In some individuals, however, diastemata may persist into adulthood.5 Etiologies are typically multifactorial, but commonly reflect discrepancies between the sizes of the teeth and dimensions of the jaw. The causes for such discrepancies are usually genetic. Other contributing etiologies may include the presence of an enlarged aberrant frenal attachment or pernicious oral habits — such as lower lip biting and digit sucking. These may cause labial flaring of the maxillary incisors, leading to a midline diastema.6,7 Also, the presence of macroglossia or tongue thrust could disrupt the delicate muscular balance in the region and force the incisors to migrate labially to reach a new equilibrium. In addition, other factors, such as a peg laterals, unerupted mesiodens, retained primary incisors, congenitally missing lateral incisors and naso-palatine cysts, may play a role in midline spacing.8

If these etiologic factors are not properly addressed during the mixed dentition phase, the diastemata may become permanent. The acceptance of the maxillary midline diastema varies greatly among individuals and has different perceptions of attractiveness in various cultures. Some consider the presence of one or more diastemata to be unesthetic and may seek closure of these spaces through orthodontic or prosthodontic means (Figure 4 and Figure 5). Consequently, oral health professionals should ask patients with diastemata to determine their esthetic preferences in the context of the functional health status of the dentition and periodontium.

FORMATION OF DIASTEMATA IN ADULTS
An acquired diastema may be a warning sign signaling advanced periodontitis. Gingival inflammation, reduced bony support and tooth mobility may contribute to the drifting of teeth — a condition called pathologic tooth migration.9 This typically affects the anterior teeth and can manifest in various forms. The most common is facial flaring of incisors, followed by rotation, extrusion, mesial or distal tipping, or a combination of these changes.10 Studies of patient populations with moderate to severe periodontitis indicate that pathologic migration is a common finding, with a prevalence ranging from 30.03% to 55.8%.10,11 Tooth migration can be disfiguring and often motivates patients to seek dental care.12


ADDITIONAL CAUSES OF PATHOLOGIC TOOTH MIGRATION
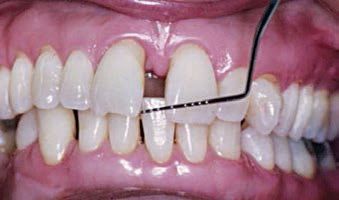
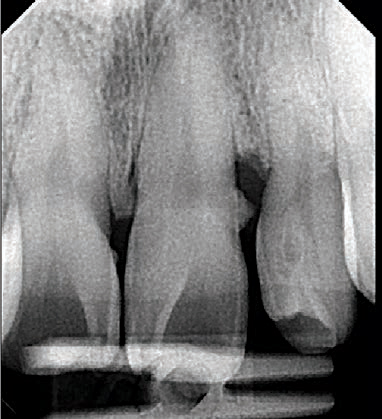
Another explanation for tooth migration is the chronic inflammatory process first proposed by Hirschfield14 in 1933. He suggested the inflamed gingiva had a higher interstitial fluid pressure due to an increase in blood flow and vascular permeability.15 According to Hirschfield, gingival inflammation and edema may increase the pressure inside the periodontal pocket, which is then transmitted to the periodontal ligament. This theory is supported, in part, by the clinical observation of a tooth tending to migrate away from its deepest pocket. This is demonstrated in Figure 7 and Figure 8, in which tooth #9 presented with a distal infrabony defect and formation of diastema on its distal.
Plaque-associated gingival overgrowth and severe inflammation or drug-induced enlargements due to phenytoin, cyclosporin A and calcium channel blockers have also been implicated in tooth displacement and acquired diastemata formation.16 Posterior bite collapse, occlusal interferences and bruxism17 also are possible etiologic factors for tooth migration. Additionally, various oral habits — such as lip and tongue habits, fingernail biting, thumb sucking, and playing wind instruments — have been associated with pathologic tooth migration.18
TREATMENT OPTIONS
key takeaways
- Etiologies for diastemata that persist in adulthood are usually multifactorial, but commonly reflect discrepancies between the sizes of the teeth and dimensions of the jaw.
- Pathologic tooth migration typically affects the anterior teeth and can manifest in various forms.
- An acquired diastema may be a warning sign of advanced periodontitis. In fact, studies of patient populations with moderate to severe periodontitis indicate that pathologic migration is a common finding.10,11
- The acceptance of the maxillary midline diastema varies greatly among individuals and has different perceptions of attractiveness — thus, dentists should ask patients with diastemata about their esthetic preferences.
- Managing moderate to severe cases of acquired diastemata may necessitate a complex and sequential intervention involving periodontic, orthodontic and prosthodontic measures.27,28
Identification of the causative factors involved in pathologic tooth migration is crucial for successful treatment. In early cases, a spontaneous correction of the tooth position has been described in several case reports following nonsurgical19,20 and surgical periodontal procedures.21-24 These cases indicate that migrated teeth sometimes return to their original positions after the etiologic factor has been eliminated (e.g., gingival inflammation, occlusal interferences or drug-induced gingival overgrowth). The return of teeth to their original positions, however, is unpredictable and depends on multiple factors. Gaumet et al25 reported the outcomes of patients with acquired anterior diastemata who underwent nonsurgical and surgical periodontal interventions. They reported a complete closure of diastemata in 51.5% of patients, while the remaining subjects exhibited various degrees of repositioning. The preoperative dimension of the diastema dictated the likelihood of its closure. Best results were noted in patients with a preoperative diastema of ≤1 mm in dimension. Rohatgi et al26 reported similar results following periodontal treatment where 32.3% of sites showed complete repositioning. They reported an inverse relationship between the severity of pathologic migration and the likelihood of spontaneous repositioning of teeth and closure of diastemata.
Managing moderate to severe cases of acquired diastemata may necessitate a complex and sequential intervention involving periodontic, orthodontic and prosthodontic measures.27,28 Such multidisciplinary approaches can be successful in restoring health, function and esthetics, but may be time-consuming and financially challenging for patients. Management of such cases typically requires periodontal therapy (nonsurgical and sometimes surgical) aimed at stabilizing the periodontium prior to orthodontic and restorative therapy. In cases of severe pathologic tooth migration, extraction of hopeless teeth with severe clinical attachment loss and mobility may be necessary to achieve optimal oral function and esthetics.
Identification of the causative factors involved in pathologic tooth migration is crucial for successful treatment
Several studies29,30 have stressed the importance of a stable and healthy periodontium before, during and after orthodontic therapy. This is because orthodontic movement in the presence of periodontitis is thought to potentially intensify periodontitis, leading to additional bone and attachment loss.
ROLE OF THE DENTAL TEAM
Clinicians should recognize pathologic tooth migration and address it with patients. If minor pathologic tooth migration appears to be the result of periodontitis, thorough scaling and root planing, and improved self-care may reverse it completely. If the migration fails to resolve, periodontal surgery as well as orthodontic and prosthetic measures may be necessary. Clinicians should stress the importance of regular maintenance visits to prevent any relapse and reappearance of the diastema, especially in patients with a history of periodontitis.
CONCLUSION
While the presence of diastemata in children is common and a normal sequela of growth and development, the formation of new diastemata in adults is not. Tooth drifting, supereruption and rotation of teeth in adults are warning signs of advanced periodontitis and are generally termed pathologic tooth migration. Identification and mitigation of all causative factors are essential to proper management of these cases.
Although the process is unpredictable, spontaneous resolution of small amounts of pathologic tooth migration is possible in mild cases after the causative factors have been removed. Moderate to severe cases of pathologic tooth migration usually necessitate a multidisciplinary approach of periodontal therapy in combination with restorative or orthodontic treatment.
References
- Taylor JE. Clinical observations relating to the normal and abnormal frenum labii superioris. Am J Orthodont Oral Surg. 1939;25:646–650.
- Gardiner JH. Midline spaces. Dent Pract Dent Rec. 1967;17:287–298.
- Weyman J. The incidence of median diastema during the eruption of the permanent teeth. Dent Pract Dent Rec. 1967;17:276–278.
- Baum AT. The midline diastema. J Oral Med. 1966;21:30–39.
- Broadbent BH: The face of the normal child (diagnosis, development). The Angle Orthodontist. 1937;7(4):183–208.
- Dewel BF. The labial frenum, midline, diastema, and palatine papilla: a clinical analysis. Dent Clin N Am. 1966;10:175–184.
- Johnson ED, Larson BE. Thumb-sucking: classification and treatment. ASDC J Dent Child. 1993;60:392–398.
- Huang WJ, Creath CJ. The midline diastema: a review of its etiology and treatment. Pediatr Dent. 1995;27:171–179.
- Chasens AI. Periodontal disease, pathologic tooth migration and adult orthodontics. N Y J Dent. 1979;49:40–43.
- Towfighi PP, Brunsvold MA, Storey AT, Arnold RM, Willman DE, McMahan CA. Pathologic migration of anterior teeth in patients with moderate to severe periodontitis. J Periodontol. 1997;68:967– 972.
- Martinez-Canut P, Carrasquer A, Magán R, Lorca A. A study on factors associated with pathologic tooth migration. J Clin Periodontol. 1997;24:492–497.
- Demetriou N, Tsami-Pandi A, Parashis A. Is it possible for periodontal patients to recognize periodontal disease? Stomatologia (Athenai). 1991;47:284–295.
- Weinstein S, Haack DC, Morris LY, Snyder BB, Attaway HE. On an equilibrium theory of tooth position. The Angle Orthodontist. 1963;33(1):1–26.
- Hirschfeld L. The dynamic relationship between pathologically migrating teeth and inflammatory tissue in periodontal pockets: A clinical study. J Periodontol. 1933;4:35–47.
- Del Fabbro M, Francetti L, Bulfamante G, Cribiu M, Miserocchi G, Weinstein RL. Fluid dynamics of gingival tissues in transition from physiological condition to inflammation. J Periodontol. 2001;72:65–73.
- Fu E, Nieh S, Wikesjö UM, Lin FG, Shen EC. Gingival overgrowth and dental alveolar alterations: possible mechanisms of cyclosporin-induced tooth migration. An experimental study in the rat. J Periodontol. 1997;68:1231–1236.
- Brunsvold MA. Pathologic tooth migration. J Periodontol. 2005;76:859–866.
- Chasens AI. Incisal guidance and the management of esthetic and dysfunctional problems. Alpha Omegan. 1980;73:43–46.
- Brunsvold MA, Zammit KW, Dongari AI. Spontaneous correction of pathologic migration following periodontal therapy. Int J Periodontics Restorative Dent. 1997;17:182–189.
- Sato S, Ujiie H, Ito K. Spontaneous correction of pathologic tooth migration and reduced infrabony pockets following nonsurgical periodontal therapy: a case report. Int J Periodontics Restorative Dent. 2004;24:456–461.
- Kumar V, SA, Thomas C. Reactive repositioning of pathologically migrated teeth following periodontal therapy. Quintessence Int. 2009;40:355–358.
- Singh J, Deshpande RN. Pathologic migration — spontaneous correction following periodontal therapy: a case report. Quintessence Int. 2002;33:65–68.
- Dadlani H, Ramachandra SS, Mehta DS. Spontaneous correction of pathologically migrated teeth with periodontal therapy alone. J Indian Soc Periodontol. 2013;17:531–534.
- Manor A, Kaffe I, Littner MM. “Spontaneous” repositioning of migrated teeth following periodontal surgery. J Clin Periodontol. 1984;11:540–545.
- Gaumet PE, Brunsvold MI, McMahan CA. Spontaneous repositioning of pathologically migrated teeth. J Periodontol. 1999;70:1177–1184.
- Rohatgi S, Narula SC, Sharma RK, Tewari S, Bansal P. Clinical evaluation of correction of pathologic migration with periodontal therapy. Quintessence Int. 2011;42:e22–e30.
- Duncan WJ. Realignment of periodontally affected maxillary teeth — a periodontist’s perspective. Part II: Case reports. N Z Dent J. 1997;93:117–123
- Oh SL. An interdisciplinary treatment to manage pathologic tooth migration: a clinical report. J Prosthet Dent. 2011;106:153–158.
- Re S, Corrente G, Abundo R, Cardaropoli D. Orthodontic treatment in periodontally compromised patients: 12-year report. Int J Periodontics Restorative Dent. 2000;20:31–39.
- Artum J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofac Orthop. 1988;93:143–148.


