
Minimal and Moderate Sedation in Pediatric Dentistry
An evidence-based overview of objectives, indications and applications for pediatric oral sedation.
The dental management of children may occasionally require advanced behavior guidance techniques, such as protective stabilization, sedation or general anesthesia.1 Parental acceptance of behavior guidance techniques has evolved over the years. Three decades ago, Murphy et al2 reported that oral sedation and general anesthesia were among the least accepted techniques. Twenty years later, Eaton et al3 found that general anesthesia had become significantly less objectionable to parents/caregivers, and was the next acceptable technique after inhalation sedation with nitrous oxide. However, oral sedation approval has improved only moderately, and is slightly more tolerated than voice control, passive restraint and the hand-over-mouth technique.3 Lawrence et al4 noted that explanation of the technique improved parental acceptance. More recently, White et al5 discovered that many parents/caregivers consider sedation as an appropriate treatment option. Nevertheless, sedation appointment scenario approval has been correlated with misconceptions.5
Contemporary trends in pediatric dentistry indicate that parents/caregivers favor care under pharmacological anxiolysis more than ever before. Minimal sedation, such as nitrous oxide, is highly accepted by parents/caregivers for potentially cooperative children, as is deep sedation/general anesthesia for uncooperative children facing extensive treatment (as these patients also need to protect their developing psyche).4–6 This article will present an overview of current indications and applications of minimal and moderate sedation in pediatric dentistry.
Minimal and moderate sedation may offer access to safe, less costly dental sedation services. It can be easily accommodated in most office settings.7–9 Under current definitions, minimal sedation is a drug-induced state in which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected. Moderate sedation is a drug-induced depression of consciousness during which patients respond purposefully to verbal commands or light tactile stimulation. No interventions are required to maintain a patent airway, spontaneous ventilation is adequate, and cardiovascular function is usually maintained.10
ORAL SEDATION REGIMENS
Dental sedation is practiced with a variety of pharmacological drug regimens by operators with varied training.1 The American Academy of Pediatric Dentistry guidelines define level of sedation by the depth of sedation achieved, not by the drug regimen used. Moreover, the guidelines state: “The caveat that loss of consciousness should be unlikely is a particularly important aspect of the definition of moderate sedation; drugs and techniques used should carry a margin of safety wide enough to render unintended loss of consciousness unlikely.”10 Subsequently, several drugs and dosages previously used for “conscious sedation” may no longer be considered an appropriate choice for minimal or moderate sedation (e.g., certain high-dose sedative-hypnotics, such as chloral hydrate).
Dental providers should be able to accurately assess the child’s developmental level, dental attitudes and temperament, and be able to anticipate the patient’s reaction to treatment. The response to oral health care may be modified by developmental delay, physical/mental disability, disease, general or situational anxiety, a previous unpleasant and/or painful dental/medical experience, inadequate preparation for the encounter, and parenting practices.11
When a child’s cognitive abilities or behavior prevent routine delivery of dental care and communicative guidance proves insufficient, the dentist must consider alternative management techniques. In some cases, referral, deferral or limited treatment may be considered. Chronic management of caries may entail periodic application of silver diamine fluoride; the silver modified atraumatic restorative technique (in which silver diamine fluoride is applied and immediately restored or sealed with conventional glass ionomer cement); interim therapeutic restorations; or the Hall technique.11–13 The decision of how to treat a pediatric patient is influenced by predoctoral dental education, society, marketing, media, communication, technology and parenting practices.14
The goals of oral sedation are to protect the patient’s safety and welfare; minimize physical discomfort and pain; control anxiety, minimize psychological trauma and maximize the potential for amnesia; control behavior and/or movement so as to allow safe completion of the procedure; and return the patient to a state in which safe discharge from medical supervision (as determined by recognized criteria) is possible.11 The objectives of minimal and moderate sedation are to place the child in a receptive state to enhance communication and cooperation. This may reduce anxiety, increase tolerance for longer appointments, aid in treatment of the mentally, physically disabled or medically compromised patient, reduce gagging, and raise the pain threshold.11
Nitrous oxide/oxygen inhalation is a common sedative that may be safely utilized to reduce anxiety and enhance communication. Its onset of action is rapid, titratable and reversible, and recovery is complete. These qualities render it ideal for minimal and moderate sedation — either as a sole sedative or titrated in combination with other agents.
APPLICATION OF MINIMAL OR MODERATE SEDATION
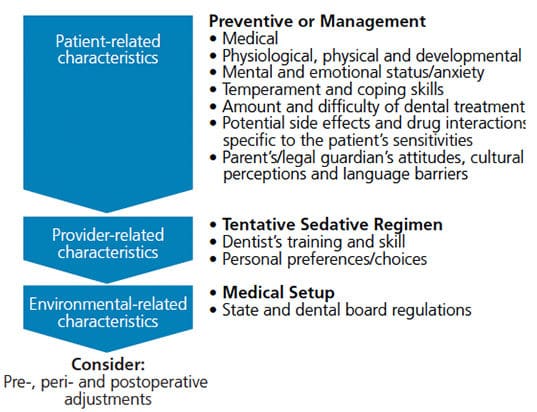
Decisions on the type of sedative regimen (medication, dosage and route) should be made based on characteristics related to the child, provider and environmental factors.
Patient-related characteristics include:
- Medical status, including the patient’s American Society of Anesthesiologists physical status classification, specific medical issues, allergies and current medication use.
- Airway examination to determine the Mallampati score and Brodsky score, and whether the patient has enlarged tonsils/adenoids, history of snoring, obstructive sleep apnea, deviated nasal septum, narrow palate, enlarged/bifid uvula, limited neck mobility, short neck, small mandible, large tongue, trismus or limited mouth opening.
- Physiological condition, such as hydration status and vital signs.
- Physical condition, based on assessment of age, weight, height, obesity, body mass index, and visible veins (for intravenous sedation).
- Mental and emotional status, as influenced by previous medical and dental experience, anxiety, hunger, general development, temperament, time of day, and coping skills.
- Amount and difficulty of dental treatment, based on assessment of the number of visits, length of expected treatment, nature of the expected treatment, and the patient’s perception of the procedure.
- Potential side effects and drug interactions, after taking into account the patient’s specific sensitivities and possible drug interactions. This may affect selection of the sedative medication, as well as dosing, and may require additional remedies or elimination of currently prescribed medications.
- Caregiver-related factors, including parental/legal guardian attitudes, cultural perceptions and language barriers.15
Provider-related characteristics include:
- Clinical training and skills; for example, the provider’s sedation permit, expertise in behavior guidance, sedation techniques, and experience with special care needs and medically compromised patients.
- Personal preferences, such as the clinician’s tolerance of misbehaving patients, and comfort with certain nonpharmacologic and pharmacotherapeutic techniques.
- Factors that may influence the type and route of sedative medication include the ability to titrate the sedative effect, therapeutic window, presence of reversal agents, duration of action, latency, onset, peak, working time, and the expected recovery time (alpha and beta half-life).
Environmental-related characteristics include:
- The medical setup, such as whether services are rendered in a private office, surgical center or hospital, and the availability of emergency backup services.
- State and specialty dental board guidelines and regulations.
With minimal and moderate oral sedation, Wright16 asserts these characteristics should be assessed in the context that “Drugs are not substitutes for the fundamental nonpharmacotherapeutic approaches to behavior guidance. Rather, they are adjuncts which can aid the dentist in providing care for some of his or her more difficult child patients.”
CHOICE OF REGIMEN
First and foremost, a tentative decision is made regarding the necessity for a preventive or management sedative regimen. Children may be categorized as those who need preventive medication and those needing management medication. Pediatric patients who need preventive medication either have abnormal responses or are unnecessarily strained by the dental situation (e.g., a timid child). By and large, minimal sedation uses agents such as nitrous oxide, diazepam, Benadryl or hydroxyzine. This may help place the child in a receptive state of mind, and enhance communication, cooperation and tolerance for longer appointments. Minimal sedation can reduce anxiety, gagging and fear of the needle. It can also raise the pain threshold and aid in treatment of the mentally, medically or physically disabled patient.11,16
Children who need management medications cannot control their behavior in the dental office. This may include patients who cannot cooperate due to a lack of psychological or emotional maturity; mental, physical or medical disability; and patients for whom the use of sedation may protect the developing psyche and/or reduce medical risk. Moderate sedation with agents such as midazolam or chloral hydrate is common. Occasionally, these agents may be combined with other drugs, such as hydroxyzine, meperidine, fentanyl or nitrous oxide.11,16 Hysterical or defiant children might need to be guided to an acceptable behavior through other behavioral and/or pharmacological techniques, such as moderate sedation, deep sedation or general anesthesia.11,16
Tentative determination of the medication regimen is based on the extent and nature of care scheduled, parent/caregiver preference and the provider’s expertise. This is related to the intrinsic properties of the medications used, such as anxiolysis, sedation, hypnosis, amnesia, analgesia, antiemesis, muscle relaxation, and other risks or benefits. Ideally the clinician should select a drug that will attend to all of the patient’s needs. The ideal sedation endpoint would be one at which the procedure can be successfully accomplished with as little distress to the patient as possible, and with cardiopulmonary stability, retention of protective airway reflexes, and age-appropriate response to verbal commands — either alone or accompanied by light tactile stimulation.15
Anxiety: When anxiety is a prominent feature, it could be beneficial to consider a mild sedative to augment alteration in perception of the dental experience for present and future appointments. With the goal of increased cooperation, using higher doses (within standard therapeutic indices) or more potent sedatives may remove inhibitions and cause overreaction to stimulus. On the other hand, when the main issue is uncooperative behavior due to lack of maturity, intellectual disability or defiance, the utilization of low-dose anxiolytics or less potent sedatives may yield a patient who overreacts to stimulus.17
Amnesia: Amnesia to control deleterious psychological consequences may be beneficial when the patient’s reaction to the sedative is not predictable (e.g., as characterized by combative uncontrolled movement, crying, or the need for active or passive protective stabilization). Benzodiazepines may produce anterograde amnesia.15,17
Analgesia: Control of pain perception may involve the use of profound local anesthesia. Opioids and nitrous oxide may elevate the pain reaction threshold. This may reduce overreaction to discomfort, such as minor painful stimuli or pressure.15,17
Muscle Relaxation and Anticonvulsant Properties: Control of untoward movement may be gained with sedative-hypnotics, such as benzodiazepines. This may be beneficial in patients with athetoid and spastic cerebral palsy.
Moderate doses of benzodiazepines affect the muscular tone, enhance inhibition of the limbic system, and provide dose dependent inhibition of the reticular activating system. Higher doses of some sedatives can induce significant inhibition of the reticular activating system (with increased risk for side effects, such as apnea, coma and death).15,17
Antiemesis: Antiemetic properties may be advantageous for children who are prone to nausea, vomiting, silent regurgitation and aspiration due to certain procedures or sensitivity to sedatives (e.g., nitrous oxide, chloral hydrate or narcotics), or due to medical issues, such as gastroesophageal reflux disease, pyloric stenosis, motion sickness, upper airway infection, asthma, cerebral palsy or Down syndrome.15
Adjustments to these tentatively selected sedatives should be established based on medical and physical characteristics specific to the patient. This risk/benefit analysis may modify the previously chosen drug regimen. In some medically compromised patients, syndromes with craniofacial abnormalities, or very young children, outpatient sedation is risky, and certain procedures must be carried out in a controlled inpatient setting to ensure safety and prevent loss of the airway. At times, moderate oral sedation may be inadvisable due to lack of ability to titrate the level of sedation and manage complications that may require intravenous access.15,18
The dentist should bear in mind that combining drugs may enhance the depth of sedation beyond the intended level and also increase side effects. Coté et al19 reported that dental specialists had the greatest frequency of negative outcomes when using three or more sedating medications. Additionally, adverse events were frequently associated with drug overdoses and interactions, particularly when three or more drugs were used.19
BALANCED APPROACH
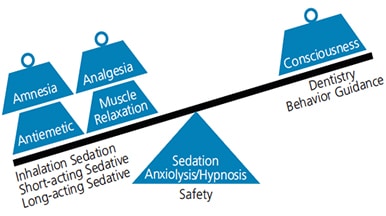
Thus, it is important for providers to strike a balance when delivering moderate oral sedation (Figure 1). Combining drugs to achieve control of anxiolysis, sedation, hypnosis, amnesia, analgesia, antiemesis and muscle relaxation may deepen the sedation beyond the intended level and increase risk of side effects. In select cases, the use of nitrous oxide and short-acting medication, along with a lower dose of a long-acting sedative, may be considered.
In order to reduce the incidence of adverse outcomes, it is imperative to adhere to published guidelines, and employ monitoring appropriate to the level of sedation provided. Staying within recommended dosages, and being familiar with the regimens utilized, are both essential to safe care. In the event of an emergency, having preset rescue systems and precalculated maximum dosages of local anesthetics and emergency/reversal medications may prevent complications and facilitate a rapid and effective response.11,20,21
Based on outcome, oral sedation plans may be modified in either of the following ways:
- Titration at the same visit is only available with nitrous oxide and/or intravenous sedatives. Additional drugs should never be re-administered by the enteral route during the same visit due to the inability to titrate oral medications.
- Utilizing the concept of “titration by appointment,” adjustments to drug selection and/or dosage may be attempted at the following visit.
Figure 2 presents an overview of the decision-making process when selecting a sedative regimen. Patient characteristics are a factor in decisions about preventive or management regimens. The components of specific drug selection should be determined based on provider-related characteristics and environmental-related characteristics. Ultimately, pre, peri or postoperative adjustment may be considered based on the sedation outcome.
KEY TAKEAWAYS
- The objectives of minimal and moderate oral sedation are to place the child in a receptive state to enhance communication and cooperation during treatment.
- Minimal sedation, such as nitrous oxide, is highly accepted by parents/caregivers for potentially cooperative children, as is deep sedation/general anesthesia for uncooperative children who face extensive treatment.4–6
- Easily accommodated in most dental offices, minimal and moderate sedation may offer access to safe and less costly dental sedation services.7–9
- Minimal sedation is a drug-induced state in which patients respond normally to verbal commands. Although cognitive function and coordination may be impaired, ventilatory and cardiovascular functions are unaffected.
- Moderate sedation is a drug-induced depression of consciousness during which patients respond purposefully to verbal commands or light tactile stimulation. No interventions are required to maintain a patent airway, spontaneous ventilation is adequate, and cardiovascular function is usually maintained.10
- Decisions on the type of sedative regimen (medication, dosage and route) should be made based on characteristics related to the child, provider and environmental factors.
REFERENCES
- Wilson S, Houpt M. Project USAP 2010: use of sedative agents in pediatric dentistry — a 25-year follow-up survey. Pediatr Dent. 2016;38:127–133.
- Murphy MG, Fields HW Jr, Machen JB. Parental acceptance of pediatric dentistry behavior management techniques. Pediatr Dent. 1984;6:193–198.
- Eaton JJ, McTigue DJ, Fields HW Jr, Beck M. Attitudes of contemporary parents toward behavior management techniques used in pediatric dentistry. Pediatr Dent. 2005;27:107–113.
- Lawrence SM, McTigue DJ, Wilson S, Odom JG, Waggoner WF, Fields HW Jr. Parental attitudes toward behavior management techniques used in pediatric dentistry. Pediatr Dent. 1991;13:151–155.
- White J, Wells M, Arheart LK, Donaldson M, Woods MA: A questionnaire of parental perceptions of conscious sedation in pediatric dentistry. Pediatr Dent. 2016;38:116–121.
- Fields HW Jr, Machen JB, Murphy MG. Acceptability of various behavior management technique relative to types of dental treatment. Pediatr Dent. 1984;6:199–203.
- Ashley PF, Williams CE, Moles DR, Parry J. Sedation versus general anesthesia for provision of dental treatment to patients younger than 18 years. Cochrane Database Syst Rev. 2015;28:CD006334.
- Ayalon S, Gozal Y, Kaufman E. The use of conscious sedation versus general anesthesia in modern dentistry: rising ethical dilemmas. Refuat Hapeh Vehashinayim (1993). 2004;21:9–26,93–94.
- Lee JY, Vann WF Jr, Roberts MW. A cost analysis of treating pediatric dental patients using general anesthesia versus conscious sedation. Anesth Prog. 2001;48:82–88.
- Coté CJ, Wilson S. American Academy of Pediatrics, American Academy of Pediatric Dentistry. Guidelines for monitoring and management of pediatric patients before during and after sedation for diagnostic and therapeutic procedures: update 2016. Pediatrics. 2016;138:pii:e20161212.
- AAPD Reference Manual, Pediatric Dentistry. 2017–2018. Available at: http://store.aapd.org/index.php/professional-resources/reference-manual.html. Accessed December 6, 2018.
- Alvear Fa B, Jew JA, Wong A, Young D. Silver modified atraumatic restorative technique (SMART): an alternative caries prevention tool. StomaEduJ. 2016;3:243–249.
- Santamaría RM, Innes NP, Machiulskiene V, Schmoeckel J, Alkilzy M, Splieth CH. Alternative caries management options for primary molars: 2.5-year outcomes of a randomised clinical trial. Caries Res. 2017;51:605–614.
- Sheller B. Challenges of managing child behavior in the 21st century dental setting. Pediatr Dent. 2004;26:111–113.
- Krauss B, Green SM. Procedural sedation and analgesia in children. Lancet. 2006;367:766–780.
- Wright ZG. Behavior Management in Dentistry for Children. Philadelphia: Saunders;1975:146–148.
- Thikkurissy S, Gosnel ES. Pain Reaction Control: Sedation. In: Nowak A, Christensen JR, Mabry TR, Townsend JA, Wells MH. Pediatric Dentistry: Infancy Through Adolescence. 6th ed. Philadelphia: Elsevier; 2019:124–126.
- Waage NS, Baker S, Sedano HO. Pediatric conditions associated with compromised airway: part 1 — congenital. Pediatr Dent. 2009;31:236–248.
- Coté CJ, Karl HW, Notterman DA, Weinberg JA, McCloskey C. Adverse sedation events in pediatrics: analysis of medications used for sedation. Pediatrics. 2000;106:633–644.
- Sapir S, Zitterell C, Kane JD. Letter to the editor. Pediatr Dent. 2017;39:94–95.
- Sapir S. Emergency airway management during moderate sedation. Decisions in Dentistry. 2018;4(6):36–39.
The author has no commercial conflicts of interest to disclose.
Featured image by LIGHTFIELDSTUDIOS/ISTOCK/GETTY IMAGES PLUS
From Decisions in Dentistry. January 2019;5(1):12–14,17.


