
Activated Irrigation in Endodontics
Compared to traditional methods, activating endodontic irrigant allows more thorough disinfection of the root canal system. While ultrasonics is a chief focus of study, the literature also supports laser-activation technologies.
One of the most cited papers on irrigation in endodontics is by Zehnder,8 who commented on the potential of newer approaches to traditional irrigation — activation of the irrigation fluid — to improve debridement of the canal system. Increasing the turbulence of the irrigant can improve penetration of the fluid to enhance antibacterial action.9 Common methods include shaking the irrigant with a file or activator tip, and use of ultrasonic and sonic tips running at a frequency to cause a hydrodynamic effect or microcavitation in the fluid. Lasers can also be used to achieve a similar effect (Figure 1). Bubbles created by these energy transfer techniques will form and collapse within the irrigant and the pressure waves will lead to shear stress along the root canal walls, which can effectively remove biofilm. This explosion and implosion of bubbles in the energized irrigant has been shown to increase fluid penetration and contact with canal walls, thereby improving cleaning efficacy.10

Lasers were first used in endodontics in 1971,11 with Nd:YAG, Er:YAG, diode and CO2 laser technologies initially used for irradiating root canals by way of heat absorption and the photodamaging effects to bacteria. The Er:YAG was found to be the more effective of the lasers utilized.11,12 The protocol introduces a laser fiber tip into the prepared root canal to the apical region to create the desired effect. This method has limitations when faced with the curved nature of canals and not being able to introduce the tip to the apical area in a narrower canal. Another disadvantage when used in a dry state is the effect on tooth structure and potential for over-enlargement or ledging of the root canal.13
CANAL CLEANING EFFICIENCY
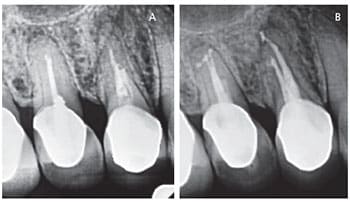
Laser-activated irrigation has since moved toward introducing the tip at an earlier stage in root canal treatment, and applying the laser to the irrigant solution to aid in cleaning the canal system (Figures 2A and 2B).14 The radiation emitted by the laser is absorbed by fluid molecules and there is an activation of the irrigant through what is described as a “transient cavitation” effect.15 Regarding cleaning efficiency, studies have shown laser-activated irrigation significantly reduces bacteria levels, with some papers demonstrating greater efficacy than other means of activation.16–19 Although there is a benefit in more effective cleaning — including smear layer removal — the disadvantage (as seen with any method of irrigant activation) is the potential for apical extrusion of the irrigant.20
Studies have since investigated placement of the laser tip, and whether it is advantageous to move the tip close to the apex (as in previous approaches) or if placement more coronally creates sufficient irrigant activation.21,22 A video setup constructed by Blanken et al21 to assess the dynamics of laser-activated irrigant showed bubble formation, with bubble expansion and subsequent collapse within the fluid due to the resulting turbulence. It was noted that bubble implosion resulting from laser activation forms secondary cavitation bubbles. In a comparison between free water and a root canal model, the authors reported that bubble formation, collapse and resultant secondary bubbles enhanced the effect. The study showed that a more coronally placed laser tip has the potential for significant irrigant activation.
Laser irradiation of the irrigant will heat the fluid and boil it to vapor in 1 microsecond. This creates the bubble, which expands. Further laser emission passes through the vapor bubble and evaporates the fluid in front of it, causing more expansion, as described by the Moses effect.23 This pushes the fluid toward the canal walls. As the laser stops, the vapor bubble shrinks and collapses, which causes shock waves within the irrigant. During this rapid irrigant flow, the rebound effect of pressure changes leads to the formation of secondary bubbles, which collapse and form smaller bubbles. This results in dynamic movement of the irrigant in what has been described as acoustic streaming.22
Matsumoto et al22 demonstrated that in a narrower root canal space the initial bubble cannot expand as much, which leads to increased streaming of the cavitation bubbles; however, there may be less energy in the shock waves created. In this study, the laser tip was not placed at a close distance to the apex and the cavitation bubbles were still able to reach the apical region. This may have applications in situations where ultrasonic activation is limited, such as in narrow canals — where laser activation may work without pre-enlarging the canal system. This can allow a more minimally invasive approach to endodontics, as the laser tip can be placed in the pulp chamber and a fully prepared or enlarged root canal is not necessary.22,24,25
EVOLVING APPROACHES
Laser-activated irrigation has evolved to include photon induced photoacoustic streaming (PIPS) and shock wave enhanced emission photoacoustic streaming (SWEEPS) technologies designed to enhance the effectiveness of laser-activated irrigation. The PIPS protocol calls for use of a special laser tip that is stripped and altered from end firing to radial firing.26 The resulting energy is emitted in multiple directions, which reportedly achieves more effective activation of the fluid — and without the potential apical extrusion of irrigants.27 This technology uses extremely low levels of energy, which leads to faster bubble collapse and a greater secondary cavitation effect, with short bursts of peak power of around 400 to 1000 watts. A study by Olivi13 demonstrated a temperature rise in the apical region of only 1.5o C after 40 seconds of use, which reduces the potential for thermal damage. Research by Peters et al28 showed the PIPS protocol to be effective in root canal disinfection.

A further literature search into PIPS yields positive results. Orinola-Zapata et al29 report PIPS significantly improved biofilm removal compared to a standard needle, sonic activation or passive ultrasonic activation. Lloyd et al30 used micro computed tomography to analyze the canal volume and debris removal using the PIPS method, and reported 2.6 times greater efficacy of debris removal than standard needle irrigation. Pedulla et al31 showed the effectiveness of the PIPS protocol in debris removal with sterile water, with or without a laser; however, the authors could not show a significant difference with sodium hypochlorite. In regard to bacterial reduction, a study of colony forming unit levels by Olivi et al32 showed significant reduction of Enterococcus faecalis using PIPS. This was also noted in systematic reviews by Sadik et al33 and Al-Aqeedi et al.34 A modified PIPS protocol was considered by Golob et al,35 who cycled between sodium hypochlorite and ethylenediaminetetraacetic acid, and lowering the energy level from 20 mJ to 10 mJ. Despite lower energy, this did not lessen the effect of PIPS in reducing bacterial levels within the canal.
The SWEEPS protocol was developed to improve the photoacoustic streaming of irrigants with PIPS (Figure 3).36 Based on a technique used with ultrasound to break kidney stones, it uses specially timed laser pulses to maximize bubble formation and collapse during irrigant activation, increasing the cleaning and debriding effects of the resulting shock waves. A study that examined bubble dynamics showed deeper penetration of bubbles with the SWEEPS protocol compared to PIPS. This finding confirmed the work of Meire et al,37 who used shorter pulses of laser irradiation to improve debris removal.
CONCLUSION
Regardless of the modality used, activated irrigation has been shown to increase the efficacy of root canal cleaning, and is evolving into the standard of care in endodontic treatment. Activation by laser has the potential to be clinically relevant because it supports minimally invasive therapy. There is a trend in endodontics toward smaller access and apical sizes38 and preserving as much tooth structure as possible, while still achieving adequate disinfection of root canals. Continued positive results in published studies may strengthen the evidence base for laser-activated irrigation.
While it is not possible to conclude there are proven benefits for laser-activated irrigation surpassing other methods, this is a developing area of endodontic disinfection that may hold promise for the future.
KEY TAKEAWAYS
- With the goal improved tooth survival, the future of endodontics is moving toward more minimally invasive, restorative-driven root canal therapy.
- Effective endodontic irrigation requires both adequate penetration of the irrigant3 and sufficient volume.7
- Increasing the turbulence of the irrigant can improve penetration of the fluid to enhance antibacterial action,9 and this has led to the development of various irrigant activation technologies.
- Common methods of activation include shaking the irrigant with a file or activator tip, use of ultrasonic and sonic tips running at a frequency to cause a hydrodynamic effect or microcavitation in the fluid, and laser activation.
- The explosion and implosion of bubbles in the energized irrigant increases fluid contact with canal walls, thereby improving cleaning efficiency.10
- Regardless of the modality used, activated irrigation has been shown to increase the efficacy of root canal cleaning, and is evolving into the standard of care in endodontic treatment.
REFERENCES
- Kojima K, Inamoto K, Nagamatsu K, et al Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:95–99.
- Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846–850.
- Chow TW. Mechanical effectiveness of root canal irrigation. J Endod.1983;9:475–479.
- Vertucci FJ. Root canal morphology and its relationship to endodontic procedures. Endod Topics. 2005;10:3–29.
- Rodig T, Hulsmann M, Muhge M, Schafers F. Quality of preparation of oval distal root canals in mandibular molars using nickel-titanium instruments. Int Endod J. 2002;35:919–928.
- Paqué F, Ganahl D, Peters O. Effects of root canal preparation on apical geometry assessed by micro-computed tomography. J Endod. 2009;35:1056–1059.
- Ram Z. Effectiveness of root canal irrigation. Oral Surg Oral Med Oral Pathol. 1977;44:306–312.
- Zehnder M. Root canal irrigants. J Endod. 2006;32:389–398.
- Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009;35:791–804.
- Dioguardi M, Di Gioia G, Illuzzi G, Laneve E, Cocco A, Troiano G. Endodontic irrigants: different methods to improve efficacy and related problems. Eur J Dent. 2018;12:459–466.
- Saydjari Y, Kupyers T, Gutknecht N. Laser application in dentistry: irradiation effects of Nd:YAG 1064 nm and diode 810 nm and 980 nm in infected root canals — a literature overview. BioMed Res Int. 2016;2016:8421656.
- Asnaashari M, Safavi N. Disinfection of contaminated canals by different laser wavelengths, while performing root canal therapy. J Lasers Med Sci. 2013;4:8–16.
- Olivi G. Laser use in endodontics: evolution from direct laser irradiation to laser-activated irrigation. J Laser Dent. 2013;21:58–71.
- de Groot SD, Verhaagen B, Versluis M, Wu K, Wesselink PR, van der Sluis LW. Laser-activated irrigation within root canals: cleaning efficacy and flow visualization. Int Endod J. 2009;42:1077–1083.
- Blanken JW, Verdaasdonk RM. Cavitation as a working mechanism of the Er,Cr:YSGG Laser in endodontics: a visualization study. J Oral Laser Appl. 2007;7:97–106.
- Cheng X, Xiang D, He W, et al. Bactericidal effect of Er:YAG laser-activated sodium hypochlorite irrigation against biofilms of Enterococcus faecalis isolate from canal of root-filled teeth with periapical lesions. Photomed Laser Surg. 2017;35:386–392.
- Cheng X, Tian T, Tian Y, et al. Erbium:yttrium aluminum garnet laser-activated sodium hypochlorite irrigation: a promising procedure for minimally invasive endodontics. Photomed Laser Surg. 2017;35:695–701.
- De Meyer S, Meire MA, Coenye T, De Moor RJ. Effect of laser-activated irrigation on biofilms in artificial root canals. Int Endod J. 2017;50:472–479.
- Race J, Zilm P, Ratnayake J, Fitzsimmons T, Marchant C, Cathro P. Efficacy of laser and ultrasonic-activated irrigation on eradicating a mixed-species biofilm in human mesial roots. Aust Endod J. 2019:doi:10.11/1/aej.12334. [Epub ahead of print].
- George R, Meyers IA, Walsh LJ. Laser activation of endodontic irrigants with improved conical laser fiber tips for removing smear layer in the apical third of the root canal. J Endod. 2008;34:1524–1527.
- Blanken J, De Moor RJ, Meire M, Verdaasdonk R. Laser induced explosive vapor and cavitation resulting in effective irrigation of the root canal. Part 1: a visualization study. Lasers Surg Med. 2009;41:514–519.
- Matsumoto H, Yoshimine Y, Akamine A. visualization of irrigant flow and cavitation induced by Er:YAG laser within a root canal model. J Endod. 2011;37:839–843.
- van Leeuwen T, van de Veen M, Verdaasdonk R, Borst C. Noncontact tissue ablation by holmium:YSGG laser pulses in blood. Lasers Surg Med. 1991;11:26–34.\
- Levy G, Rizoiu L, Friedman S, Lam H. Pressure waves in root canals induced by Nd:YAG laser. J Endod. 1996;22:81–84.
- Ahmad M, Pitt Ford TR, Crum LA, Walton AJ. Ultrasonic debridement of root canals: acoustic cavitation and its relevance. J Endod. 1988;14:486–493.
- Arslan H, Capar D, Saygili G, Gok T, Ackay M. Effect of photon–initiated photoacoustic streaming on removal of apically placed dentinal debris. Int Endod J. 2014;47:1072–1077.
- Peeters H, Suardita K, Mooduto L, Gutknechtd. Extrusion of irrigant in open apex teeth with periapical lesions following laser-activated irrigation and passive ultrasonic irrigation. Iran Endod J. 2018;13:169–175.
- Peters O, Bardsley S, Fong J, Pandher G, Divito E. Disinfection of root canals with photon-initiated photoacoustic streaming. J Endod. 2011;37:1008–1012.
- Ordinola‐Zapata R, Bramante C, Aprecio R, Handysides R, Jaramillo D. Biofilm removal by 6% sodium hypochlorite activated by different irrigation techniques. Int Endod J. 2014;47:659–666.
- Lloyd A, Uhles JP, Clement DJ, Garcia-Godoy F. Elimination of intracanal tissue and debris through a novel laser-activated system assessed using high-resolution micro-computed tomography: a pilot study. J Endod. 2014;40:584–587.
- Pedulla E, Genovese C, Campagna E, Tempera G, Rapisarda E. Decontamination efficacy of photon-initiated photoacoustic streaming (PIPS) of irrigants using low-energy laser settings: an ex vivo study. Int Endod J. 2012;45:865–870.
- Olivi G, DiVito E, Peters O, et al. Disinfection efficacy of photon-induced photoacoustic streaming on root canals infected with Enterococcus faecalis: an ex vivo study. J Am Dent Assoc. 2014;145:843–848.
- Sadik B, Arikan S, Beldüz N, Yaşa Y, Karasoy D, Cehreli M. Effects of laser treatment on endodontic pathogen Enterococcus faecalis: a systematic review. Photomed Laser Surg. 2013;31:192–200.
- Al-Aqeedi M, Mohammed S, Rasheed R. Evaluating the antibacterial effect of low powered laser activated irrigation on Enterococcus faecalis infected root canals. Int J Enhan Res Sci Tech Engineering. 2015;3:243–250.
- Golob B, Olivi G, Vrabec M, El Feghali R, Parker S, Benedicenti S. Efficacy of photon-induced photoacoustic streaming in the reduction of Enterococcus faecalis within the root canal: different settings and different sodium hypochlorite concentrations. J Endod. 2017;43:1730–1735.
- Lukac N, Muc BT, Jezersek M, Lukac M. Photoacoustic endodontics using the novel SWEEPS Er:YAG laser modality. J Laser Health Academy. 2017;1:1–7.
- Meire MA, Havelaerts S, De Moor RJ. Influence of lasing parameters on the cleaning efficacy of laser-activated irrigation with pulsed erbium lasers. Lasers Med Sci. 2016;31:653–638.
- Mukherjee P, Patel A, Chandak M, Kashikar R. Minimally invasive endodontics a promising future concept: a review article. Int J Sci Stud. 2017;5:245-251.
The author has no commercial conflicts of interest to disclose.


