
Vital Pulp Therapy for Primary Molars
This clinical approach can be a useful option for treating deep caries in deciduous molars with vital pulp.
PURCHASE COURSE
This course was published in the September 2016 issue and expires 09/30/19. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the factors involved in pulpal diagnosis in primary teeth.
- Compare and contrast a pulpotomy with indirect pulp treatment in primary molars.
- Discuss the options of final restoration for primary molars in which vital pulp therapy has been performed.
An intact, functional primary dentition plays a critical role in a child’s oral health, as it ensures a smooth transition to the permanent dentition. For this reason, it is important (whenever possible) to preserve primary teeth with deep caries until their natural exfoliation. While restorative or surgical management of caries in primary teeth is straightforward, treating deep caries lesions in vital teeth with possible pulpal involvement can be challenging. Vital pulp therapy focuses on treating the pulp with the hopes of retaining its vitality, rather than performing root canal treatment in which the pulp is fully removed. Pulpotomy and indirect pulp treatment (IPT) are the most common vital pulp therapies for managing deep caries in the primary dentition. This article will discuss assessment of pulpal status, as well as the key principles of pulpotomies and IPT in deciduous teeth.
Successful management of deep caries lesions begins with an accurate pulpal diagnosis. Such a diagnosis can be achieved after the patient’s history of symptoms and clinical and radiographic findings have been reviewed. Assessing the pulpal status of primary teeth can be the most difficult part of vital pulp therapy. There are three reasons why diagnosis can be challenging. First, the diagnostic tools used in adult endodontic diagnosis are not reliable in primary teeth. Second, determining an accurate pulpal diagnosis based on clinical signs and symptoms is nearly impossible without a histological examination. Third, a detailed medical and dental history is necessary for an accurate diagnosis, but children are not reliable providers of such information. Both the pediatric patient and parent/caregiver need to be questioned about the child’s symptoms. Although it is possible for a tooth with extensive disease to present without any history of pain, this sensation is usually associated with pulpal inflammation.1 While pain generated by a stimulus typically means minor and reversible inflammatory changes, spontaneous pain usually indicates extensive degenerative changes that have extended into the root canal. As such, teeth with a history of spontaneous pain are not candidates for vital pulp therapy.1,2
Besides a history of pain, soft tissue changes, pathological mobility and percussion sensitivity should also be evaluated during a clinical examination. A sinus tract or alveolar abscess is a sign of a necrotic pulp, in which case vital pulp therapy is inappropriate (Figure 1). The presence of tooth mobility beyond the level of what’s seen during normal exfoliation is also a contraindication for vital pulp therapy. Although percussion sensitivity can be a sign of a necrotic pulp, the reliability of a child’s response to this test is questionable. Moreover, the possibility of causing pain during percussion testing may frighten a pediatric patient.2 For this same reason, pulp vitality testing (e.g., a cold test) is also not typically used on primary teeth.
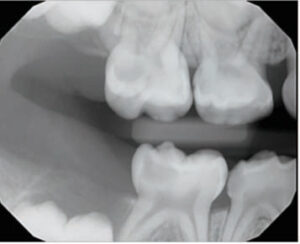
High-quality radiographs are needed for an accurate diagnosis. In primary molars, pathological changes are most often apparent in the furcation areas (Figure 2). The loss of lamina dura and decreased radiopacity of the bone in the furcation area are among the first signs of necrotic or dying pulps (Figure 3).2 Pathological external or internal root resorption are also signs of advanced pulpal pathoses. Bitewings provide the most accurate assessment of the depth of the caries lesion, its proximity to the pulp, and furcation changes. Taking bitewings on young children to capture furcation areas can be difficult, however. In these cases, selected periapical radiographs should be captured on teeth with deep caries. The superimposition of developing permanent teeth and palatal roots in the furcation area may hinder visibility and make accurate observation of subtle changes to maxillary primary molars difficult.1,2



The placement of a glass ionomer interim therapeutic restoration prior to vital pulp therapy may support the pulpal diagnosis.3–5 Interim therapeutic restorations are placed at the initial examination in large cavitated lesions with questionable pulpal status without using local anesthesia or rubber dams. Before the restoration is applied, superficial caries material should be removed with hand instruments or large, slow-speed round burs.3–5 The tooth should subsequently be reevaluated in four weeks to three months. At reevaluation, if the tooth remains clinically and radiographically normal, the pulp is considered to be vital or reversibly inflamed, and vital pulp therapy can be performed. If clinical or radiographic signs or symptoms of advanced pulpal inflammation are present during the observation period, the pulpal damage is irreversible, and extraction or pulpectomy therapy is indicated.4,5 This approach may be particularly helpful in determining the pulpal status of teeth with deep interproximal caries.5 Following the observation period, if the pulp appears normal or reversible pulpitis is present, a pulpotomy or IPT should be considered. Studies have shown that both therapies have similar indications and outcomes.4,6–9
PULPOTOMIES
Traditionally, when caries removal in primary teeth results in a carious/mechanical pulpal exposure, a pulpotomy is performed.9 During this procedure, the coronal pulp is amputated and the remaining radicular pulpal tissue is assessed and treated with a pulp medicament. Afterward, the coronal pulp chamber is filled with a suitable base, and the tooth is restored using a well-sealed restoration.9 All decayed dentin should be removed before entering the pulp chamber in order to minimize the risk of bacterial contamination. A bleeding pulp inside the pulp chamber indicates a vital pulp. If the pulp chamber is empty or purulent, the pulpotomy should be terminated and a pulpectomy or extraction must be performed.2
Removing all residual hemorrhaging coronal pulp tissue tags hidden underneath the pulp horn is important for controlling bleeding and accurately accessing the pulp’s status. Once the coronal pulp is removed using a large, slow-speed round bur or sharp spoon, a damp cotton pellet is used with gentle pressure to control hemorrhaging from the pulp stumps. If hemostasis can be achieved within several minutes, the radicular tissue is thought to be vital (Figure 4) and the tooth is a good candidate for a pulpotomy. If there is excessive hemorrhaging that cannot be controlled, the tooth is no longer a candidate for vital pulp therapy, and nonvital pulp therapy or extraction is indicated. When the hemorrhaging is controlled, a pulpotomy medicament — such as formocresol, ferric sulfate or mineral trioxide aggregate (MTA) — should be applied.
Formocresol is the most commonly used pulpotomy agent.10,11 Although safety concerns have been raised because it contains formaldehyde,11 no correlation between formocresol pulpotomies and cancer has been demonstrated.12 The amount of formocresol used in a pulpotomy is minimal, and, when used prudently, formocresol is a safe, economical and effective pulp medicament.12 Studies have shown, however, that the clinical success of a formocresol pulpotomy decreases with time.3,4 Ferric sulfate offers a nonformaldehyde option for clinicians concerned about the safety of formocresol, and this agent offers success rates similar to formocresol.13
By comparison, MTA offers improved biocompatibility and performs as well as or better than formocresol and ferric sulfate.14 While it may become the preferred pulpotomy agent in the future, MTA’s high cost and risk of tooth discoloration have limited its use thus far.15 In recent years, MTA-like products with similar properties have been introduced, providing clinicians with more affordable choices — although long-term clinical studies on the effectiveness of these products are needed.
INDIRECT PULP TREATMENT
This therapeutic approach involves covering a small amount of caries that is left in place (to avoid pulpal exposure) with a biocompatible material, such as calcium hydroxide or glass ionomer, and then restoring the tooth with a restoration that seals the tooth from microleakage.2,9 Clinically, IPT works by removing the superficial layer of carious dentin while leaving a small layer of affected dentin that contains a minimal amount of pathogenic microorganisms. The caries lesion is then sealed. When this therapy goes as planned, the caries is arrested, affected dentin remineralizes, and tertiary dentin forms inside the pulp chamber.16–18 Reentry is not required for primary molars.18
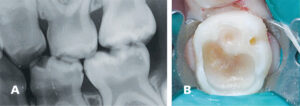
When performing IPT, all lateral walls must be excavated to sound dentin, and only a small amount of caries located over the pulp is allowed to remain (Figures 5A and 5B). A sound understanding of the internal anatomy of primary teeth helps practitioners avoid overly aggressive caries removal, thus reducing the risk of pulpal exposure.19,20 A slow-speed handpiece with a large, round bur is recommended to provide controlled tissue excavation.2
In long-term studies, IPT has shown higher success rates than pulpotomies.9 The technique offers many advantages, including preventing direct pulp injuries, maintaining pulp integrity, and avoiding pulpal tissue exposure to potentially toxic chemicals. This approach also allows shorter treatment time, and there is no need to reenter. Even so, pulpotomy remains the more commonly used technique. Although an accurate pulpal diagnosis is critical to the success of IPT, achieving this in pediatric patients can be challenging. Other barriers include the historical success of pulpotomies, clinicians’ confidence in its outcomes, and inadequate reimbursement for this procedure.21
Modern caries management in primary teeth has evolved from surgical approaches with complete caries removal to a less invasive approach, with partial or no caries removal underneath restorations.20,22 The Hall technique is an example of the latter, and studies demonstrate its success.23,24 In this technique, a stainless steel crown (SSC) is placed over carious primary molars using a glass ionomer cement. This is done without caries removal, tooth preparation or local anesthesia.24 In a randomized control trial with a five-year follow-up, sealing caries with the Hall technique statistically and clinically outperformed conventional intracoronal restorations.22,25 The Hall crown, however, is not suitable for every child or every molar with a caries lesion.26 First, the Hall crown should only be fitted on a tooth that is at low (or no) risk of irreversible pulpal pathology. Second, Hall crowns require careful follow-up after fitting, and prompt management is indicated if pulpal pathology arises. In addition, very young or anxious children may not be able to cope with the crown fitting.
FINAL RESTORATION
Besides an accurate preoperative diagnosis, a final restoration that provides a complete biological seal is critical to the success of vital pulp therapy.2,9 Traditionally, SSCs have been the restorative choice for primary molars. More recently, parents/caregivers often prefer tooth-colored restorations.27 Veneered SSCs have been introduced as an esthetic alternative to traditional SSCs, but chipped facing is a possibility over the long term.28,29 In addition, significantly more tooth structure must be removed to fit these crowns — thus, the risk of accidental pulpal exposure increases during tooth preparation.28
Resin-based composite is another esthetic restorative option for primary molars. Studies on the use of composite restorations in primary molars treated with pulpotomies and IPT have shown promising results, particularly on teeth with occlusal restorations.7,8 The most common reason for resin restoration failure is coronal microleakage. The risk of coronal microleakage increases with the number of surfaces involved.29,30 New esthetic, full-coverage options, such as zirconia crowns, are also available. Although they provide excellent esthetics, their effects on pulp treatment, surrounding tissue, and opposing natural teeth need long-term observation.
FOLLOW-UP CARE

Clinical and radiographic examinations should be performed every six months on teeth treated with vital pulp therapy.9 Treatment is considered clinically successful when there are no clinical signs or symptoms of advanced pulp degeneration. Bitewings capturing the furcation area or periapical radiographs can be compared with preoperative radiographs to evaluate changes over time. Ideally, no change should be observed between preoperative and follow-up radiographs of successfully treated teeth. However, changes in root canals may be noted. Internal resorption and pulp canal obliteration are two commonly seen changes.2 Minor and self-limiting internal resorption can be monitored with no intervention required. That said, internal resorption can also be progressive and destructive, even perforating the canals and involving surrounding bone. In this case, vital pulp therapy has failed and intervention, such as extraction, is indicated.31 Pulp canal obliteration involves the natural narrowing of canals over time (Figure 6); this is a sign of pulpal healing and is considered a treatment success.
CONCLUSION
Primary molars with deep caries can be managed with vital pulp therapy. Both pulpotomies and IPT are suitable treatments for pulp that is healthy or has reversible inflammation. The success of vital pulp therapy depends on accurate pulpal diagnoses, careful operative practices, well-sealed restorations and appropriate follow-up care.
References
- Camp JH. Diagnosis dilemmas in vital pulp therapy: treatment for the toothache is changing, especially in young, immature teeth. J Endod. 2008;34(Suppl 7):S6–S12.
- Seale NS, Coll JA. Vital pulp therapy for the primary dentition. Gen Dent. 2010;58:192–194.
- Vij R, Coll JA, Shelton P, Farooq NS. Caries control and other variables associated with success of primary molar vital pulp therapy. Pediatr Dent. 2004;26:214–220.
- Coll JA. Indirect pulp capping and primary teeth: is the primary tooth pulpotomy out of date? J Endod. 2008;34(Suppl 7):S34–S39.
- Coll J, Campbell A, NI C. Effects of glass ionomer temporary restorations on pulpal diagnosis and treatment outcomes in primary molars. Pediatr Dent. 2013;45:416–421.
- Farooq NS, Coll JA, Kuwabara A, Shelton P. Success rates of formocresol pulpotomy and indirect pulp therapy in the treatment of deep dentinal caries in primary teeth. Pediatr Dent. 2000;22:278–286.
- Falster CA, Araujo FB, Straffon LH, Nör JE. Indirect pulp treatment: in vivo outcomes of an adhesive resin system vs calcium hydroxide for protection of the dentin-pulp complex. Pediatr Dent. 2002;24:241–248.
- Casagrande L, Bento LW, Dalpian DM, García-Godoy F, De Araujo FB. Indirect pulp treatment in primary teeth: 4-year results. Am J Dent. 2010;23:34–38.
- American Academy of Pediatric Dentistry Clinical Affairs Committee — Pulp Therapy Subcommittee; American Academy of Pediatric Dentistry Council on Clinical Affairs. Guideline on pulp therapy for primary and young permanent teeth. Pediatr Dent. 2015;37(Spec Issue 6):244–252.
- Dunston B, Coll JA. A survey of primary tooth pulp therapy as taught in U.S. dental schools and practiced by diplomates of the American Board of Pediatric Dentistry. Pediatr Dent. 2008;30:42–48.
- Walker LA, Sanders BJ, Jones JE, et al. Current trends in pulp therapy: a survey analyzing pulpotomy techniques taught in pediatric dental residency programs. J Dent Child (Chic). 2013;80:31–35.
- Milnes AR. Is formocresol obsolete? A fresh look at the evidence concerning safety issues. J Endod. 2008;34(Suppl 7):40–46.
- Peng L, Ye L, Guo X, et al. Evaluation of formocresol versus ferric sulphate primary molar pulpotomy: a systematic review and meta-analysis. Int Endod J. 2007;40:751–757.
- Peng L, Ye L, Tan H, Zhou X. Evaluation of the formocresol versus mineral trioxide aggregate primary molar pulpotomy: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e40–e44.
- Agamy HA, Bakry NS, Mounir MMF, Avery DR. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr Dent. 2004;26:302–309.
- Ribeiro CCC, de Oliveira Lula EC, da Costa RCN, Nunes AMM. Rationale for the partial removal of carious tissue in primary teeth. Pediatr Dent. 2012;34:39–41.
- Ferreira JMS, Pinheiro SL, Sampaio FC, de Menezes VA. Caries removal in primary teeth — a systematic review. Quintessence Int. 2012;43:e9–e15.
- Wambier DS, dos Santos FA, Guedes-Pinto AC, Jaeger RG, Simionato MRL. Ultrastructural and microbiological analysis of the dentin layers affected by caries lesions in primary molars treated by minimal intervention. Pediatr Dent. 2007;29:228–234.
- Orhan AI, Oz FT, Orhan K. Pulp exposure occurrence and outcomes after 1- or 2-visit indirect pulp therapy vs complete caries removal in primary and permanent molars. Pediatr Dent. 2010;32:347–355.
- Ricketts D, Lamont T, Innes NPT, Kidd E, Clarkson JE. Operative caries management in adults and children. Cochrane Database Syst Rev. 2013;3:CD003808.
- Seale NS, Glickman GN. Contemporary perspectives on vital pulp therapy: views from the endodontists and pediatric dentists. J Endod. 2008;34:261–267.
- Innes NP, Evans DJP, Stirrups DR. Sealing caries in primary molars: randomized control trial, 5-year results. J Dent Res. 2011;90:1405–1410.
- Innes NP, Stirrups DR, Evans DJP, Hall N, Leggate M. A novel technique using preformed metal crowns for managing carious primary molars in general practice — a retrospective analysis. Br Dent J. 2006;200:451–454.
- Innes NP, Evans DJ, Stirrups DR. The Hall Technique; a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice: acceptability of the technique and outcomes at 23 months. BMC Oral Health. 2007;7:18.
- Innes NP, Stewart M, Souster GED. The Hall Technique; retrospective case-note follow-up of 5-year RCT. Br Dent J. 2015;219:395–400.
- Innes NP, Evans DJP. Modern approaches to caries management of the primary dentition. Br Dent J. 2013;214:559–566.
- Zimmerman J, Feigal R, Till M, Hodges J. Parental attitudes on restorative materials as factors influencing current use in pediatric dentistry. Pediatr Dent. 2009;31:63–70.
- Ram D, Fuks AB, Eidelman E. Long-term clinical performance of esthetic primary molar crowns. Pediatr Dent. 2003;25:582–584.
- Guelmann M, Shapira J, Silva DR, Fuks AB. Esthetic restorative options for pulpotomized primary molars: a review of literature. J Clin Pediatr Dent. 2011;36:123–126.
- Guelmann M, McIlwain MF, Primosch RE. Radiographic assessment of primary molar pulpotomies restored with resin-based materials. Pediatr Dent. 2005;27:24–27.
- Huth KC, Paschos E, Hajek-Al-Khatar N, et al. Effectiveness of 4 pulpotomy techniques — randomized controlled trial. J Dent Res. 2005;84:1144–1148.
From Decisions in Dentistry. September 2016;2(09):33–36.




