Treating Dental Trauma
Appropriate diagnosis and a timely response will improve outcomes when managing traumatic dental injuries.
In many cases of traumatic dental injuries, the timeliness of care is key to saving the tooth. It is thus important for all dentists to have an understanding of how to diagnose and treat the most common dental injuries — and this is especially critical in the emergency phase of treatment. Proper management of dental trauma is most often a team effort, with general dentists, pediatric dentists, periodontists or oral surgeons on the front line of the emergency service, and endodontic specialists joining the effort to preserve the tooth with respect to the pulp, pulpal space and root. An informed and coordinated effort will ensure the patient receives the most effective care.
A panel of experts from the American Association of Endodontists (AAE) prepared an updated version of Guidelines for the Treatment of Traumatic Dental Injuries.1,2 These guidelines were based, in part, on the recommendations of the International Association of Dental Traumatology (see iadt-dentaltrauma.org for more information). This article provides an overview of the AAE guidelines, and clinicians can download the complete guidelines at aae.org/clinical-resources/ trauma-resources.aspx.
The benefit of adhering to guidelines when treating dental trauma was demonstrated in a study by Bucher et al.3 Compared to cases treated sans guideline compliance, the researchers noted that cases that adhered to guidelines produced more favorable outcomes — including significantly lower complication rates. The study also found that early follow-up visits were essential to ensure prompt treatment of complications when they arose.3
EMERGENCY CARE
Prior to any treatment, clinicians must evaluate the injury thoroughly by careful clinical and radiographic investigation. It is recommended to follow a checklist to ensure that all necessary information regarding the patient and injury is gathered, including:
- Patient’s name, age, sex, address and contact numbers (include weight for young patients)
- Central nervous system symptoms exhibited after the injury
- Patient’s general health
- When, where and how the injury occurred
- Treatment the patient received elsewhere
- History of previous dental injuries
- Disturbances in the bite
- Tooth reactions to thermal changes or sensitivity to sweet and sour
- If the teeth are sore to the touch or when eating
- If the patient is experiencing spontaneous pain in the teeth
Once this information is gathered, a diagnosis can be made and appropriate treatment rendered. If the injured individual is not a patient of record, all necessary demographic information should be gathered as soon as the patient arrives and prior to any assessment. In the case of avulsion and the tooth being out of its socket, the clinician should immediately place the tooth in a physiological solution of specialized media (such as an appropriate salt solution) or milk, or saline if these are not available. Only after the tooth is secured in solution should the clinician obtain the patient’s information. Once the patient is seated in the dental chair, it is necessary to do a quick central nervous system (CNS) evaluation before proceeding with further assessment.
Often, the dentist is the first health care provider to see the patient after a head injury (any dental trauma is, by definition, a head injury), and he or she must assess the risk of concussion or hemorrhage. It has been estimated by a meta-analysis that the prevalence of intracranial hemorrhage after a mild head injury is 8%, and the onset of symptoms can be delayed for minutes to hours.4 The most common signs of serious cerebral concussion or hemorrhage are loss of consciousness or post-traumatic amnesia. Nausea/vomiting, fluids from the ear/nose, situational confusion, blurred vision or uneven pupils, and difficulty of speech and/or slurred speech may also indicate serious injury.5
Once the patient has been cleared of any CNS issues, the dental trauma should be assessed. The key is to obtain comprehensive information about the injury and, to do so, oral health professionals must conduct thorough extraoral and intraoral clinical exams, as well as appropriate radiographic evaluations.
The current AAE guidelines recommend taking one occlusal and two periapical radiographs with different lateral angulations for all dental injuries, including crown fractures. If cone beam computed tomography is available, it should be considered for more serious injuries, such as crown/root, root and alveolar fractures, as well as all luxation injuries.
Additionally, sensitivity tests should be conducted on all teeth involved, including opposing teeth. Cold testing is recommended over electric pulp testing in young patients.6 Both testing methods should be considered, however, especially when there is no response to one of the two. The pulp might be nonresponsive for several weeks after a traumatic injury, so a pulp test should be done at every follow-up appointment until a normal response is obtained.7
Once the diagnosis is confirmed and more serious complications — such as CNS issues and jaw or other facial bone fractures — have been ruled out, clinicians should initiate the emergency phase of treatment. The aim of therapy should be to either maintain or regain pulpal vitality in traumatized teeth. This is because dental trauma most frequently occurs in preteens or young teens in whom the teeth have not yet fully developed, and root development will cease without a vital pulp.
CLINICAL EXAMPLES
Dental trauma can be roughly divided into two groups: fractures and luxation injuries. Fractures are further divided by type: crown, crown-root and root fractures. If the pulp is exposed to the oral environment, it is considered as a complicated fracture; if not exposed, it is an uncomplicated fracture.



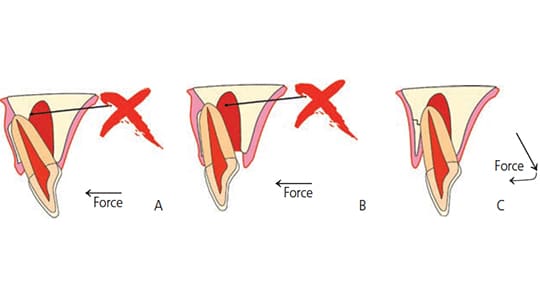
Crown Fractures: The first thing to do in any crown or crown-root fracture is to look for the broken tooth fragment. With modern bonding technology, it may be possible to rebond the fragment to the tooth, which is the best solution esthetically. Prior to reattaching the fragment, the remaining dental thickness immediately covering the pulp should be assessed radiographically and clinically. If at least 0.5 mm of the dentin remains, there is no need to cover it with a protective liner. If the remaining dentin is less than 0.5 mm, however, it is advisable to cover the deepest part (closest to the pulp) with a cavity liner, and dimple the fragment accordingly.8,9 If the tooth fragment was kept dry, it should be rehydrated in distilled water or saline for 30 minutes prior to reattachment. This process will increase its bonding strength10 (Figures 1A through 1C).
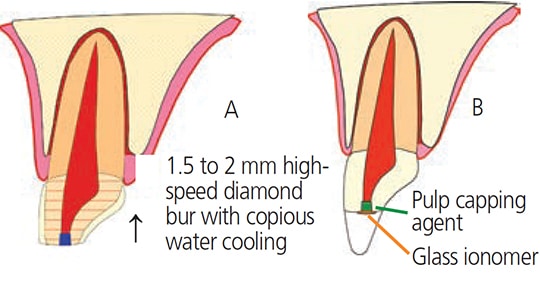
The goal in a complicated fracture is to create a bacteria-tight seal to protect the pulp, but only after ensuring the pulpal wound is clean and all inflamed tissue has been removed.11,12 The two best capping materials available are calcium hydroxide and mineral trioxide aggregate,13,14 although newer bioceramic materials are showing promise for this application. It is advisable to create a 1- to 2-mm reservoir into the pulp using a high-speed diamond bur and copious water cooling, followed by placement of the capping material; the tooth fragment is either reattached or the crown restored with a composite resin material (Figures 2A through 2C).
Crown-Root Fractures: This is one of the more challenging fractures to treat because the fracture margin has to be exposed around the tooth/crown in order to properly restore the tooth. This can be accomplished by gingivectomy if the fracture line is in the sulcus. In more extreme cases, the tooth will need to be extruded with orthodontic forces or surgically repositioned. In the emergency session, if the pulp is exposed, it must be protected in the same fashion as in a complicated crown fracture. If it is not exposed, all accessible exposed dentin areas should be covered for the patient’s comfort.
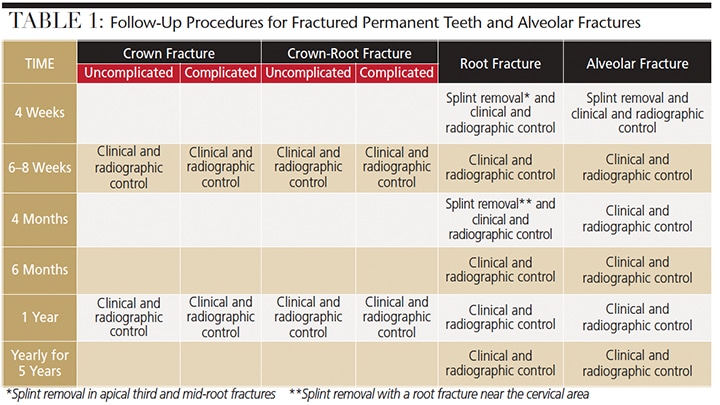
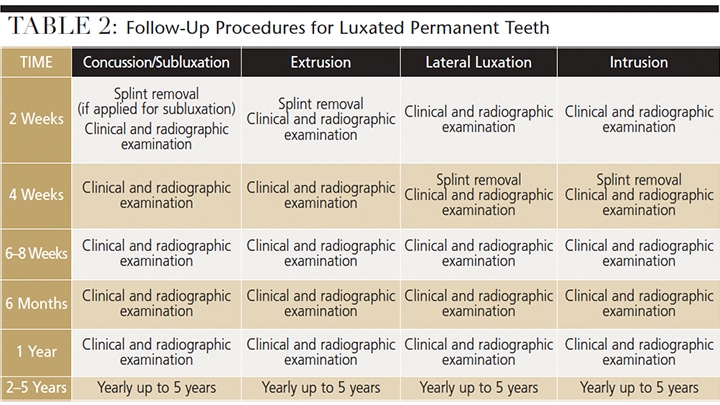
Pulpal survival for all of these fracture types is generally good; however, endodontic treatment may be indicated later.15,16 It is of utmost importance, therefore, that a recall schedule is followed and that any teeth involved in the trauma are tested every time. Table 1 and Table 2 outline the recommended recall rates for most common dental injuries. It is not uncommon for there to be no response to vitality tests for up to three months, and a lack of response to vitality tests does not always indicate that root canal treatment is needed — especially in young and immature teeth. Clinicians are advised to look for at least one other sign of pulpal necrosis, such as vestibule swelling, periapical lesions and/or dramatic color change of the crown. If no signs exist, continue to monitor the patient every three months for up to 12 months.
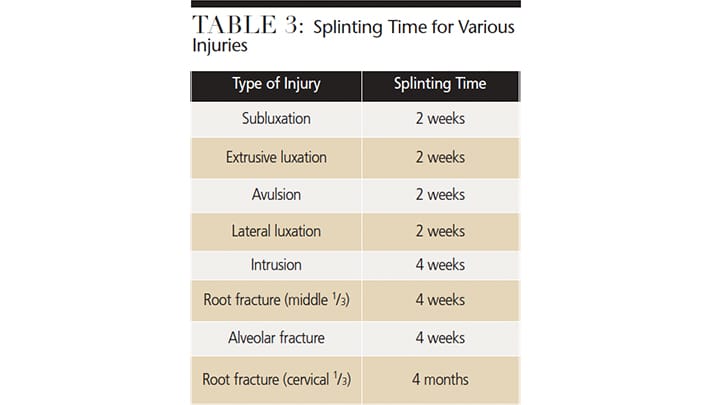
Root Fractures: Although the pulp is affected in all root fractures, if the fragments are approximated soon after the fracture, there is a good chance that endodontic treatment may not be necessary. Observation is warranted, however. With good approximation, it is likely the pulp will revascularize across the fracture, regardless of the patient’s age17,18 (Figures 3A through 3F). In two retrospective studies that included assessment of splinting type and time of root fracture, it was determined that if the cervical portion of the tooth is stable once the two pieces have been approximated, the best treatment outcomes are obtained without a splint or utilizing a flexible splint for two weeks.2,18 Longer splinting time is only recommended when the fracture is close to the cervical area.


Luxation Injuries: All luxation injuries will cause some damage to the periodontal ligament (PDL) and, in some cases, the pulp, as well. The immediate treatment is to limit further damage to the PDL and allow for the best possible healing. As with all dental injuries, follow-up is essential. Late complications, such as internal or external root resorptions, are relatively frequent and require endodontic treatment, especially in more severe injuries. In many cases, referral to an endodontist is advisable.
Luxation injuries are divided into subcategories, mainly by degree of severity. The two mildest are termed “concussion” and “subluxation.” In these cases, the tooth is still in its original location, but is tender to percussion and/or — in the case of subluxation — shows increased mobility. While no immediate treatment is needed for these injuries, follow- up is critical because the pulp may become necrotic, making endodontic intervention paramount.
frequently pushed through the cortical plate facially (A). In order to reposition the tooth, it has to be released prior to moving the crown forward (B and C). SCHEMATIC ILLUSTRATIONS COURTESY ASGEIR SIGURDSSON, DDS, MS
When trauma has moved the tooth out of its normal position, it needs to be replaced gently as soon as possible. The only exceptions are cases of intrusion in which it might not be possible or advisable to manipulate the tooth immediately. When an immature tooth is intruded up to 7 mm, it is recommended to wait three weeks and watch for signs of reeruption. If no signs exist, the clinician can initiate orthodontic repositioning. For intrusion of more than 7 mm, surgical or orthodontic repositioning should be performed within three weeks. In the case of an intruded tooth with a closed apex, there is a possibility of reeruption if the tooth is slightly intruded (less than 3 mm) and the patient is younger than 17 years old. If the tooth is not moving after two to three weeks, however, orthodontic extrusion or extraction and reimplantation is recommended. If a tooth with a closed apex is intruded more than 3 mm, orthodontic or surgical repositioning should be performed within three weeks. The risk with all intrusions is that the intruded tooth may ankylose in the infraposition. Once this begins, the tooth may not be movable — except possibly surgically. The patient and parents/guardians should be advised the long-term prognosis of an intruded tooth is unpredictable, as it is likely to eventually be lost due to ankylosis.19–21

Splinting of a luxated tooth is only recommended for teeth that are still mobile after repositioning. In all types of trauma cases, a splint must allow for physiological movement22,23 regarding splinting time (Figures 4A through 4C, Figure 5 and Table 3).
When assessing luxation trauma, it is important to consider the maturity of the apex. If it is still open, there is a chance the pulp will survive the trauma or revascularize, allowing continued tooth growth (Figures 6A through 6C). If the apex is closed, endodontic treatment is likely warranted. It is advisable to follow the patient closely (Table 1) or refer him or her to an endodontist for further evaluation. Due to the injury of the PDL, rapid inflammatory root resorption can occur — within days or a few weeks — if the necrotic pulpal tissue becomes infected. For mature teeth diagnosed with necrotic pulps, placing calcium hydroxide for two to four weeks prior to obturation is recommended; however, clinicians should allow the PDL to heal for two weeks before placement (see the avulsion treatment discussion). Apexification or revascularization is recommended for teeth with open apices.24,25



It is important to remember that dental injuries do not always fall into one group or category, but often a combination of categories, and that injuries involving multiple categories will impact the outcome. For example, it was recently demonstrated the existence of a concurrent luxation injury with an uncomplicated crown fracture and complete root development are significant risk factors for pulp necrosis.26
Avulsion: Time outside of the socket for an avulsed tooth is the most critical factor in its survival. If the tooth is replanted within 30 minutes, or, alternately, kept in a physiological solution of specialized media or milk for a few hours, it has a fairly good prognosis.27,28 If the tooth has been dry for more than 60 minutes, the PDL cannot be expected to survive and the tooth will likely become ankylosed (Figure 7). Once reimplanted, most teeth need to be stabilized with a physiological splint for two weeks.29

structure is lost and replaced by bone. Note that no apparent periodontal ligament
space is evident.
If the avulsed tooth has an open apex and was reimplanted within the hour, there is a possibility the pulp will revascularize. In this case, delaying endodontic treatment at the emergency stage is recommended. Endodontic treatment should only be performed later if signs of pulpal necrosis, root resorption and/or arrested root development are confirmed.
In the case of a closed apex, revascularization is not expected. Therefore, endodontic treatment must be initiated two weeks after the tooth is reimplanted, and prior to removal of the splint. Treatment should not be initiated earlier, as any further manipulation of the tooth prior to, or immediately after, reimplantation can cause further damage to the PDL. In addition, it has been shown that placing calcium hydroxide as an intracanal medicament immediately after reimplantation will promote inflammation that can lead to PDL damage.30 If the tooth had been kept dry longer than 60 minutes, performing root canal treatment prior to replantation is indicated.31
After the emergency situation has been managed and the tooth or teeth stabilized, the second phase begins, in which the pulpal condition and likelihood of root resorption have to be carefully evaluated, and the patient followed over a period of months, if not years. Developing a follow- up timeline is essential to allow for intervention if signs of complications appear. In such cases, an endodontist’s expertise plays an important role because diagnosing, preventing and treating pulpal complications are integral components of endodontic training, as are pulp regeneration and treating inflammatory root resorption (Figures 8A and 8B).

CONCLUSION
Traumatic dental injuries present difficult challenges for patients and dentists. Current evidence allows dental professionals to manage situations that, in the past, often resulted in crippled dentition and unsightly appearance. Appropriate treatment can turn what at first glance looks like a hopeless situation into a very satisfactory outcome for patients. The endodontic specialist can play an important role in the team approach to treating patients with traumatic dental injuries.
KEY TAKEAWAYS
- When treating traumatic dental injuries, the timeliness of care is critical to saving the tooth.
- Proper management of dental trauma is most often a team effort, with general dentists, pediatric dentists, periodontists or oral surgeons on the front line of the emergency service, and endodontists joining the effort to preserve the tooth with respect to the pulp, pulpal space and root.
- Compliance with accepted dental trauma treatment guidelines has been show to improve outcomes.3
- While dental trauma can be roughly divided into fractures and luxation injuries, it is important to remember that injuries do not always fall into one group or category — but often a combination of categories.
- Proper and timely follow-up is essential when managing all dental injuries.
REFERENCES
- Diangelis AJ, Andreasen JO, Ebeleseder KA, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2–12.
- Andreasen JO, Ahrensburg SS, Tsilingaridis G. Root fractures: the influence of type of healing and location of fracture on tooth survival rates — an analysis of 492 cases. Dent Traumatol. 2012;28:404–409.
- Bucher K, Neumann C, Thiering E, Hickel R, Kuhnisch J. Complications and survival rates of teeth after dental trauma over a 5-year period. Clin Oral Invest. 2013;17:1311–1318.
- Hofman PA, Nelemans P, Kemerink GJ, Wilmink JT. Value of radiological diagnosis of skull fracture in the management of mild head injury: meta-analysis. J Neurol Neurosurg Psych. 2000;68:416–422.
- McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport, Zurich, November 2012. J Athl Train. 2013;48:554–575.
- Fuss Z, Trowbridge H, Bender IB, Rickoff B, Sorin S. Assessment of reliability of electrical and thermal pulp testing agents. J Endod. 1986;12:301–305.
- Skieller V. The prognosis for young teeth loosened after mechanical injuries. Acta Odonta Scand. 1960;18:171–173.
- About I, Murray PE, Franquin JC, Remusat M, Smith AJ. The effect of cavity restoration variables on odontoblast cell numbers and dental repair. J Dent. 2001;29:109–117.
- Murray PE, About I, Lumley PJ, Franquin JC, Windsor LJ, Smith AJ. Odontoblast morphology and dental repair. J Dent. 2003;31:75–82.
- Capp CI, Roda MI, Tamaki R, Castanho GM, Camargo MA, de Cara AA. Reattachment of rehydrated dental fragment using two techniques. Dent Traumatol. 2009;25:95–99.
- Cox CF, Bergenholtz G, Fitzgerald M, et al. Capping of the dental pulp mechanically exposed to the oral microflora — a 5-week observation of wound healing in the monkey. J Oral Path. 1982;11:327–339.
- Cvek M, Lundberg M. Histological appearance of pulps after exposure by a crown fracture, partial pulpotomy, and clinical diagnosis of healing. J Endod. 1983;9:8–11.
- Cvek M. A clinical report on partial pulpotomy and capping with calcium hydroxide in permanent incisors with complicated crown fracture. J Endod. 1978;4:232–237.
- Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25:197–205.
- Andreasen FM, Noren JG, Andreasen JO, Engelhardtsen S, Lindh-Stromberg U. Longterm survival of fragment bonding in the treatment of fractured crowns: a multicenter clinical study. Quintessence Int. 1995;26:669–681.
- Robertson A, Andreasen FM, Andreasen JO, Noren JG. Long-term prognosis of crown-fractured permanent incisors. The effect of stage of root development and associated luxation injury. Int J Paedi Dent. 2000;10:191–199.
- Zachrisson BU, Jacobsen I. Long-term prognosis of 66 permanent anterior teeth with root fracture. Scan J Dent Res. 1975;83:345–354.
- Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7–17 years. Dent Traumatol. 2008;24:379–387.
- Alkhalifa JD, Alazemi AA. Intrusive luxation of permanent teeth: a systematic review of factors important for treatment decision-making. Dent Traumatol. 2014;30:169–175.
- Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth. Part 2. A clinical study of the effect of preinjury and injury factors, such as sex, age, stage of root development, tooth location, and extent of injury including number of intruded teeth on 140 intruded permanent teeth. Dent Traumatol. 2006;22:90–98.
- Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth. Part 3. A clinical study of the effect of treatment variables such as treatment delay, method of repositioning, type of splint, length of splinting and antibiotics on 140 teeth. Dent Traumatol. 2006;22:99–111.
- Kahler B, Heithersay GS. An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent Traumatol. 2008;24:2–10.
- Andreasen JO, Andreasen FM, Mejare I, Cvek M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol. 2004;20:203–211.
- Huang GT. A paradigm shift in endodontic management of immature teeth: conservation of stem cells for regeneration. J Dent. 2008;36:379–386.
- Trope M. Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin N Am. 2010;54:313–324.
- Wang C, Qin M, Guan Y. Analysis of pulp prognosis in 603 permanent teeth with uncomplicated crown fracture with or without luxation. Dent Traumatol. [Epub ahead of print]: 2014.
- Blomlof L, Lindskog S, Hedstrom KG, Hammarstrom L. Vitality of periodontal ligament cells after storage of monkey teeth in milk or saliva. Scand J Dent Res. 1980;88:441–445.
- de Souza BD, Bortoluzzi EA, da Silveira Teixeira C, Felippe WT, Simoes CM, Felippe MC. Effect of HBSS storage time on human periodontal ligament fibroblast viability. Dent Traumatol. 2010;26:481–483.
- Hinckfuss SE, Messer LB. Splinting duration and periodontal outcomes for replanted avulsed teeth: a systematic review. Dent Traumatol. 2009;25:150–157.
- Lindskog S, Blomlof L, Hammarstrom L. Cellular colonization of denuded root surfaces in vivo: cell morphology in dentin resorption and cementum repair. J Clin Perio. 1987;14:390–395.
- Day P, Duggal M. Interventions for treating traumatised permanent front teeth: avulsed (knocked out) and replanted. Cochrane Database Syst Rev. 2010;1:CD006542.
A version of this article originally appeared in ENDODONTICS: Colleagues for Excellence, Summer 2014. Reused with permission from the American Association of Endodontists, ©2014. The AAE clinical newsletter is available at aae.org/colleagues.
Featured photo by DEFUN/ISTOCK/THINKSTOCK
From Decisions in Dentistry. January 2017;3(1):28-33.