
Therapeutic Approaches to Erosive Tooth Wear
Use these evidence-based techniques to prevent and treat this common oral health condition.
As the consumption of acidic beverages continues to increase in developed nations, erosion and tooth wear are increasingly common threats to oral health. The acidic nature of soft drinks and similar beverages, flow rate (or frequency of consumption), and choice of artificially sweetened beverages are correlated with dental erosion.1 Once the outer layer of enamel has broken down, the dentition is not able to rebuild a new enamel surface. When the surface structure is compromised, secondary dentin is more likely to form, and the tooth eventually becomes less responsive to stimuli.
This loss of tooth structure puts oral health at risk and negatively impacts quality of life by leading to dentinal hypersensitivity. The availability of a relatively new measuring and recording tool — and the advent of a “person-centric” approach to care — may help dental providers improve outcomes for patients experiencing hypersensitivity.
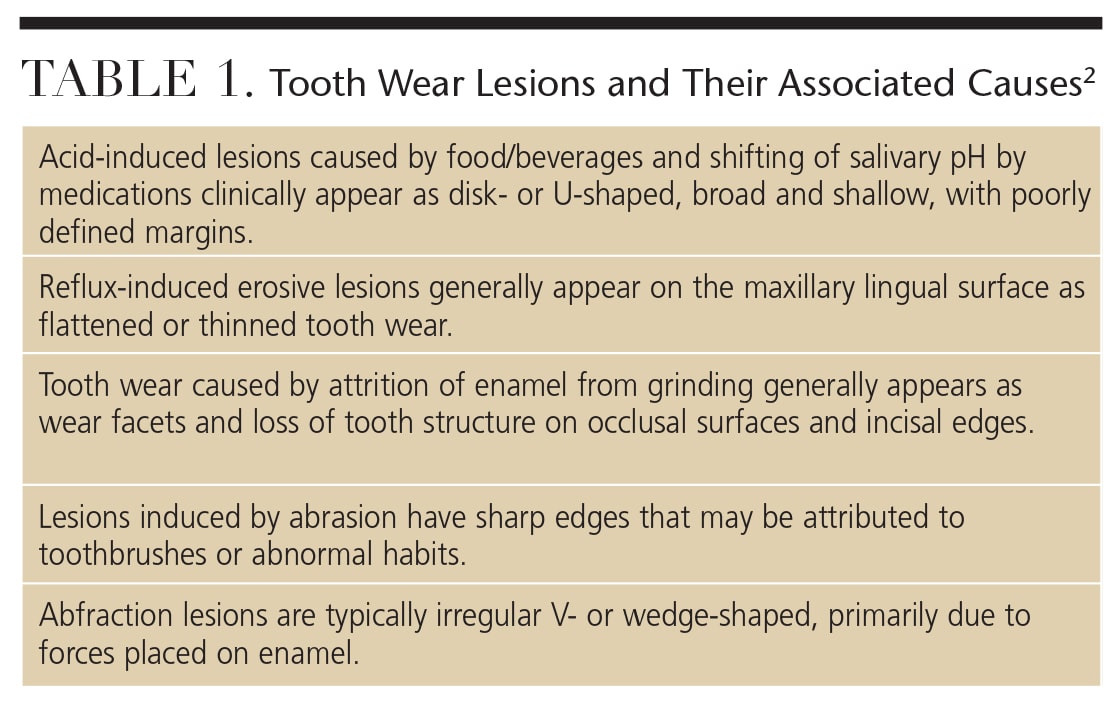
Dentinal hypersensitivity describes a decrease in enamel thickness, thereby initiating a potential sensation through a nerve fibril encased in the dental tubule. Table 1 lists tooth-wear lesions and their associated causes.2 A leading origin of dentinal sensitivity is erosion — a form of tooth wear caused by repeated short exposures of insults, such as acids. These acids may result from intrinsic (e.g., gastroesophageal reflux disease, bulimia or anorexia) or extrinsic sources (such as diet, drug use and oral hygiene factors). In the presence of acidic challenges, the combined role of erosion and abrasion may increase wear.3–5
Erosion is also dependent on host susceptibility, such as low enamel quality, thin enamel surface, salivary factors, gingival recession, exposure of cervical dentin, and/or the acidity of the oral environment.6 In this paper, the term “tooth wear” will include noncarious cervical lesions (NCCL).2 There are four distinct factors that contribute to tooth wear: erosion (loss of tooth structure caused by acids); attrition (mechanical loss of tooth structure caused by tooth-to-tooth contact); abrasion (mechanical loss of tooth structure caused by contact with other materials); and abfraction (dynamic tooth wear caused by the combination of compressive forces).2,7
TOOL FOR MEASURING TOOTH WEAR
Erosion reduces structural integrity, pulpal vitality and esthetics. Men typically experience erosion more often than women.8 Differences exist in the diagnosis and assessment between scales used to record prevalence information; thus, data across different studies may not be entirely comparable.9
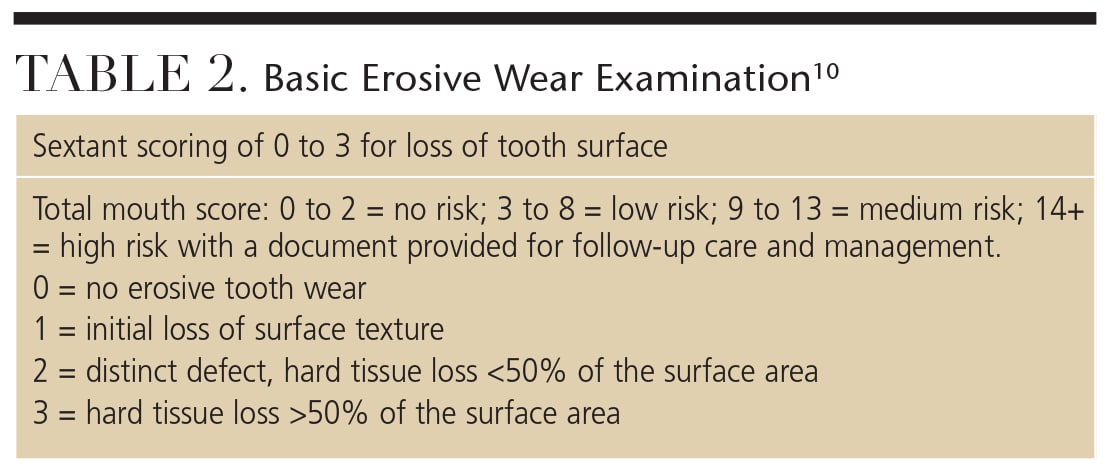
In 2008, Bartlett et al10 published the Basic Erosive Wear Examination (BEWE), which ranks tooth wear by sextant from 0 to 3, summing up the total area of tooth loss (on a scale that goes to 18), and ranking the extent of risk from none to high (Table 2). Once a determination of risk has been made, a support guide helps clinicians educate patients about individual risk scores, and informs them about intrinsic, extrinsic and susceptibility risk factors. Designed as a tool to help develop a standardized index of tooth wear, the BEWE may help oral health professionals place more emphasis on erosive wear, and assist their patients in preventing or managing this oral health threat.10
PERSON-CENTRIC CARE
Person-centric care is inclusive of both disease management and health. An individual spends a very short time as a “patient,” and the term describes the person as subservient to treatment, prevention and management. The evolution from patient-centered to person-centered care represents a shift from a disease management approach to a health-oriented model. Person-centric care involves engaging individuals in the context of their physical and social environments to make self-determined choices.11 Individuals maintain ultimate responsibility for their own health. In disease treatment models, patients are passive recipients of care, with providers making decisions about their needs.
Dental professionals have the unique opportunity to serve as oral health coaches for people experiencing dental erosion. As guides, dental providers may describe and educate people about prevention, and explain the various treatment strategies from which patients can choose. Of course, a thorough assessment must first be conducted in order to identify patient needs.
Patient engagement includes initiating a conversation about oral care habits in which information may be shared between clinicians and patients. For example, when clinicians explain how a desensitizing toothpaste works, they can reference two methods of action:
- Potassium ions navigate the dentinal tubule to reach the cell body (odontoblast) within the pulp to depolarize the nerve. Subsequent use of the toothpaste keeps the nerve depolarized to limit nerve transmission upon tooth stimulation.
- Potassium nitrate occludes dentinal tubules on the tooth surface.
The individual’s responsibility is to adapt his or her oral care routine to prevent further breakdown and deterioration of enamel and/or dentin. If a person maintains the integrity of the tooth, the viability of the pulp is maintained and further breakdown can be prevented. Apoptosis, or programmed cell death related to overstimulation, can be limited. This is important because enamel is necessary to protect the pulp from overstimulation. If the pulp develops secondary dentin, it reduces the tooth’s ability to respond to sensation and may make the tooth more susceptible to further pulpal breakdown.
The first step in guiding person-centric care is the needs assessment, in which an oral screening is conducted and tooth wear identified. The degree to which the various factors interplay should be assessed at an individual level by measuring the depth and width of the tooth wear, and asking about sensitivity. Using a pain scale may be helpful.12 In addition, clinicians may benefit from using a tool such as the BEWE to screen and track tooth wear. Bartlett10 recommends screening every two years for low-risk individuals, and every six months to 12 months for medium- to high-risk individuals. Progression of wear is measured using impressions, study casts or images, and/or by charting the depth and width of lesions.
PREVENTION OF NONCARIOUS CERVICAL LESIONS
Until the underlying cause of tooth wear is controlled, progression will likely continue. According to Pecie et al,13 there is a lack of evidence on how best to prevent NCCLs, and further study is needed in regard to effective preventive strategies. The primary goal is to eliminate the source of the erosion, such as the consumption of acidic foods and beverages (e.g., sports drinks, energy drinks, juice and soft drinks).14
Anticipatory guidance for individuals at risk of tooth wear involves a thorough dietary analysis, taking medical and dental histories to determine internal and external acidic sources, and identifying a patient’s susceptibility. Nutritional counseling is beneficial to address external sources of acids in the diet. Additionally, harm-reduction strategies — such as use of an antacid rinse to increase oral pH after an acidic exposure — help reduce enamel softening.15,16 To reduce abrasion, toothbrushing should be avoided after an acidic challenge. Brushing pressure is also associated with increased risk of tooth wear.17 Reducing pressure applied with the toothbrush and recommending soft toothbrushes and minimally abrasive dentifrices may help reduce risk. Toothbrushes are now available with sensors to indicate when excess pressure is applied during brushing.
Traditional preventive strategies focus on preservation of tooth structure through remineralization. Fluoride therapy may be recommended. Numerous products can be used to reduce sensitivity, including (but not limited to) fluoride toothpaste, fluoride rinses, in-office fluoride treatments (gel or varnish), calcium phosphate technologies (for use in the dental office, as well as at home), 5% glutaraldehyde and 35% hydroxyethyl methacrylate, bonding adhesives, arginine-calcium carbonate in-office paste, potassium nitrate toothpastes, and potassium oxalate strips. Educational approaches include improved brushing techniques, comprehensive oral hygiene instructions, recommendation of an improved self-care routine, and prescription of an occlusal guard to reduce occlusal stress.
key takeaways
- Factors contributing to tooth wear include erosion, attrition, abrasion and abfraction.2,7
- Anticipatory guidance for individuals at risk of tooth wear involves a thorough dietary analysis, taking medical and dental histories to determine internal and external acidic sources, and identifying a patient’s susceptibility.
- Once a determination of risk has been made, clinicians can use support guides to help educate patients about risk factors and preventive approaches that involve both professional and home care.
- The evolution from “patient-centered” care to “personcentric” care involves engaging individuals in the context of their physical and social environments to make selfdetermined choices.11
MANAGEMENT AND TREATMENT OF TOOTH WEAR
Tooth wear is challenging to treat (e.g., restoration failure has been cited in the literature,)18 and there remains controversy over whether it needs to be treated.19 Bartlett et al5 recommends treatment only in high-risk groups. Traditionally, glass-ionomer-based materials were the treatment of choice when tooth wear required intervention. A review of the literature, however, suggests that resin-based composite (RBC) is indicated due to its excellent esthetic properties and clinical performance.18 Concern over esthetics is another reason people seek treatment for tooth wear. Clinically significant issues associated with these lesions include dentinal hypersensitivity, plaque retention, structural integrity of the area, and pulpal vitality.
To address each person’s needs — and determine the best treatment options — clinicians must consider the individual’s personal and environmental characteristics. A study by the Practitioners Engaged in Applied Research and Learning (PEARL) Practice-Based Translational Network looked at using person-centric care in individuals with tooth wear and dentinal hypersensitivity.19 The PEARL researchers examined the uses of a potassium nitrate dentifrice, RBC restorations and sealants in a randomized, comparative effectiveness study of NCCLs in subjects who reported baseline sensitivity of 3 or higher (on a scale of 0 to 10). The six-month study found that sealants and RBC restorations proved equally effective in reducing dentinal hypersensitivity for most participants, and that the relative ease of application of the sealant (compared to a restoration) might save considerable time in treating NCCLs. In addition, the use of a dentifrice to reduce hypersensitivity was not as effective as a sealant or restoration.18
In low-risk cases, experts recommend less invasive preventive methods rather than treatment with irreversible dental procedures.5 Applying sealants for individuals with painful NCCLs is an additional option that may reduce time and cost to patients. In high-risk sensitivity cases (as determined by the BEWE score), restorative therapies, such as RBC, may be indicated.
CONCLUSION
Dental providers are uniquely positioned to reduce the burden of oral disease by screening for, and educating patients about, tooth wear. With myriad educational interventions and treatment strategies available, dental professionals can make a difference in reducing the risk of tooth wear and erosion, and effectively addressing dentinal hypersensitivity issues with their patients.
References
- Gravelle BL, Hagen Ii TW, Mayhew SL, Crumpton B, Sanders T, Horne V. Soft drinks and in vitro dental erosion. Gen Dent. 2015;63(4):33–38.
- Terry DA, McGuire MK, McLaren E, Fulton R, Swift EJ Jr. Perioesthetic approach to the diagnosis and treatment of carious and noncarious cervical lesions: Part I. J Esthet Restor Dent. 2003;15:217–232.
- Moazzez R, Bartlett D, Anggiansah A. Dental erosion, gastro-oesophageal reflux disease and saliva: how are they related? J Dent. 2004;32(6):489–494.
- Brown RE, Morisky DE, Silverstein SJ. Meth mouth severity in response to drug-use patterns and dental access in methamphetamine users. J Calif Dent Assoc. 2013;41(6):421–428.
- Bartlett DW, Shah P. A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85:306–312.
- Wood I, Jawad Z, Paisley C, Brunton P. Non-carious cervical tooth surface loss: a literature review. J Dent. 2008;36:759–766.
- Grippo JO. Noncarious cervical lesions: the decision to ignore or restore. J Esthet Dent. 1992;(Suppl4):55–64.
- McGuire J, Szabo A, Jackson S, Bradley TG, Okunseri C. Erosive tooth wear among children in the United States: relationship to race/ethnicity and obesity. Int J Paediatr Dent. 2009;19:91–98.
- Bartlett D, Phillips K, Smith B. A difference in perspective — the North American and European interpretations of tooth wear. Int J Prosthodont. 1999;12:401–408.
- Bartlett D, Ganss C, Lussi A. Basic Erosive Wear Examination (BEWE): a new scoring system for scientific and clinical needs. Clin Oral Investig. 2008;12(Suppl1):S65–S68.
- Curro FA, Robbins DA, Millenson ML, Fox CH, Naftolin F. Person-centric clinical trials: an opportunity for the good clinical practice (GCP)-practice-based research network. J Clin Pharmacol. 2013;53:1091–1094.
- Orchardson R, Gillam DG. Managing dentin hypersensitivity. J Am Dent Assoc. 2006;137:990–998.
- Pecie R, Krejci I, Garcia-Godoy F, Bortolotto T. Noncarious cervical lesions — a clinical concept based on the literature review. Part 1: prevention. Am J Dent. 2011;24:49–56.
- U.S. Food and Drug Administration. Acidified and Low-Acid Canned Foods: Approximate pH of Foods and Food products. Available at: foodscience.caes.uga.edu/extension/documents/fdaapproximatephoffoodslacf-phs.pdf. Accessed March 10, 2016.
- Turssi CP, Vianna LM, Hara AT, do Amaral FL, França FM, Basting RT. Counteractive effect of antacid suspensions on intrinsic dental erosion. Eur J Oral Sci. 2012;120:349–352.
- Alves Mdo S, Mantilla TF, Bridi EC, Basting RT, França FM, Amaral FL, Turssi CP. Rinsing with antacid suspension reduces hydrochloric acid-induced erosion. Arch Oral Biol. 2016;61:66–70.
- Brandini D, de Sousa A, Trevisan C, et al. Noncarious cervical lesions and their association with toothbrushing practices: in vivo evaluation. Oper Dent. 2011;36:581–589.
- Lee WC, Eakle WS. Stress-induced cervical lesions: review of advances in the past 10 years. J Prosthet Dent. 1996;75:487–494.
- Veitz-Keenan A, Barna JA, Strober B, et al. Treatments for hypersensitive noncarious cervical lesions: a Practitioners Engaged in Applied Research and Learning (PEARL) Network randomized clinical effectiveness study. J Am Dent Assoc. 2013;144:495–506.


