
Risk-Based Treatment Planning
Oral health risk assessment helps support comprehensive, personalized therapy that contributes to better care and optimal outcomes.
PURCHASE COURSE
This course was published in the February 2017 issue and expires February 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Explain the concept of risk-stratified care management, and its practical implementation in dental practice.
- Discuss the most common uses for risk-based treatment planning, and the role therapy and intervention play in determining overall health.
- List disease indicators and other risk factors that should be considered during patient assessment and care.
- Identify the types of practice settings most often associated with use of caries risk assessment tools, and effective strategies for positively influencing patient behavior in regard to oral health.
A common methodology employed within oral health disease management is risk-stratified assessment and treatment. As explained by the American Academy of Family Physicians, “Risk-stratified care management (RSCM) is the process of assigning a health risk status to a patient, and using the patient’s risk status to direct and improve care. The goal of RSCM is to help patients achieve the best health and quality of life possible by preventing chronic disease, stabilizing current chronic conditions, and preventing acceleration to higher-risk categories and higher associated costs.”1 In dentistry, risk assessment is most commonly used to evaluate caries or periodontal disease activity, and serve as a foundation for care goals and patient communication. In many offices and clinics, dental hygienists are a primary driver of caries risk management implementation, as research indicates that more than 98% of dental hygienists believe risk assessment is a key part of their practice.2 Given the emergence of risk-stratified care delivery, this article will review risk-assessment methodologies, practice characteristics and workflow implementation.
Oral health risk assessment aids care teams in understanding the probability of oral disease development, and prospects for changes in the disease process due to protective, behavioral and/or clinical interventions.3–5 Identifying patient-specific disease indicators and risk factors provides a basis to determine the patient’s risk status, usually signified as low, moderate or high.3,6 This information is documented and shared with the patient to establish an individual care program.3,7
CARIES RISK ASSESSMENT
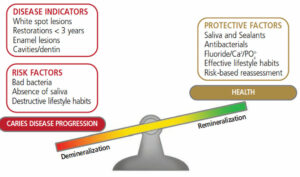
Featherstone et al8–10 propose that caries risk is assessed in two phases. The first determines an individual’s indicators of disease, inherent risk factors, and if protective factors provide any mitigation. The second determines level of risk, during which a clinician’s professional judgment documents the patient’s status via chart notation and CDT code entry (D0601, low caries risk; D0602, moderate caries risk; and D0603, high caries risk). The new D0600 code can also be used if a nonionizing procedure capable of quantifying, monitoring and recording changes in tooth structure/mineralization is administered. As seen in Figure 1, risk factors and disease indicators will tip the balance of the oral environment toward caries disease, while protective factors are associated with improved oral health (e.g., remineralization versus demineralization). The presence of disease indicators is associated with high risk, and an elevated number of risk factors typically indicates higher risk. An analysis by Bader et al11 demonstrates the disease indicators most often related to moderate or high caries risk include multiple restorations, gross cavitation of teeth, plaque/calculus accumulation, and exposed root surfaces.
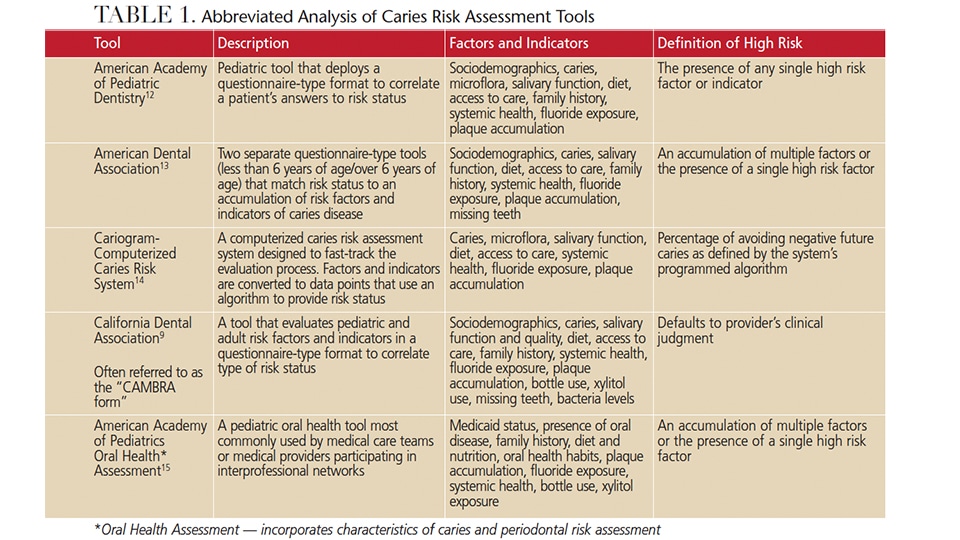
In an analysis of risk assessment by dentists involved in the Dental Practice- Based Research Network, participants were asked to rate the importance of caries risk factors in treatment planning.3 Oral hygiene, diet and nutrition, salivary function, patient knowledge and commitment to health were ranked as key factors. Various tools have been developed to assist practitioners in assessing oral health characteristics and determining risk (Table 1).9,12–15 These consist of forms or templates that list a series of questions or statements to be answered for further evaluation and assignment of risk status. Given that definitive research in caries risk and prognosis is lacking, professional consensus on the best of these tools does not exist, and provider preference most often dictates which tool is used.16
PERIODONTAL RISK ASSESSMENT
Like caries, the evaluation of periodontal risk also includes weighing disease indicators, as well as risk and protective factors.17 The disease indicators most often associated with higher risk include attachment loss, furcation involvement, missing teeth, bone height, plaque/calculus accumulation, pocket depth and bleeding on probing.17–19 As a means to systematically evaluate periodontal risk, the World Workshop on Periodontics recommends evaluating factors within seven groups: genetic influencers, systemic health, health behaviors/lifestyle, access to care, socioeconomic status, psychological profile and disease etiology.17,20–22 The health conditions most often associated with high risk status are diabetes and/or smoking.17,19,23–25 Although there is agreement on the ability of periodontal risk assessment tools to predict disease progression, there is no consensus about the best available tool. As with caries assessment, the tool selected for periodontal analysis usually depends on provider preference and the patient populations receiving care. Table 2 provides an abbreviated summary of periodontal risk assessment tools.19,23–27
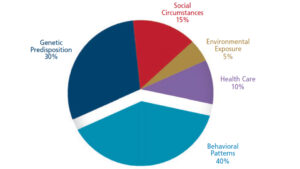
 It is worth noting that dental professionals administering periodontal or caries risk assessments list nonbiologic factors — including health behaviors, environment and oral health prioritization — as key drivers in risk status.3,17,20–22 This is supported by an American Academy of Pediatric Dentistry Pediatric Oral Health Research and Policy Center report, which notes these factors may result in higher disease risk, even if biologic risk factors are not observed. The report goes on to state, “Any model of caries-risk assessment must address both the biologic and behavioral management of the disease.”28 This methodology focuses on primary and secondary prevention, as well as the determinants of health.
It is worth noting that dental professionals administering periodontal or caries risk assessments list nonbiologic factors — including health behaviors, environment and oral health prioritization — as key drivers in risk status.3,17,20–22 This is supported by an American Academy of Pediatric Dentistry Pediatric Oral Health Research and Policy Center report, which notes these factors may result in higher disease risk, even if biologic risk factors are not observed. The report goes on to state, “Any model of caries-risk assessment must address both the biologic and behavioral management of the disease.”28 This methodology focuses on primary and secondary prevention, as well as the determinants of health.
![risk-table-2]() DETERMINANTS OF HEALTH
DETERMINANTS OF HEALTH
There are multiple determinants of health outcomes, and several interconnected factors that influence individual health. As seen in Figure 2, treatment and intervention by clinicians impact approximately 10% of total health determinants.29–32 Clinicians’ effective use of risk assessment tools will help patients achieve health goals, and facilitate individualized care plans that encourage buy-in from care teams and patients. In turn, this will help influence patient behavior — which represents approximately 40% of health determinants.3,32
Various approaches have been proposed to modify behavior, with the majority of models focusing on conveying the perceived benefits of behavior change, and understanding an individual’s self-efficacy.33 The goal is to meet the patient on his or her level, create an understanding of risk factors and risky behavior, and develop a shared conclusion that protective behaviors can offset or mitigate disease risk. The most effective strategies for influencing behavior and achieving patient buy-in include goal setting, establishing processes for monitoring challenges and opportunities, cooperative planning and motivational interviewing (MI).33–36 The latter has been advocated as a tool to activate behavior transformation via constructive conversation.37–40 This process allows patients to lead the conversation by conveying what is important to them. In turn, the provider should support patient preferences and align these choices with appropriate health goals.
By eliminating guilt concepts, patient blame, and the feeling of an individual as unacceptable, the MI approach creates a positive interpersonal environment for change without the mandate for it to occur automatically.37,41 One of the cornerstones of MI is that individuals are “experts” about themselves, and they will make independent decisions regarding health and lifestyle.37,41 In comparison to standard instruction and routine care, studies have found the use of MI produces improvement in plaque indices and gingival health.37,42–44 In addition, a recent systematic review concluded that MI has the potential to help patients with poor oral health, and that MI training could be useful for dental professionals.37 As most analyses focus on the short-term impact of MI, further research is warranted on the long-term implications of MI in oral health care.
RISK ASSESSMENT IN PRACTICE
The literature on practice-level use of risk assessment is limited and commonly focuses on caries risk assessment (CRA). Francisco et al2 report that 29% of responding clinicians (n=216) used an established form to complete CRA (71% did not use any form). Per the Francisco study, the American Academy of Pediatric Dentistry tool12 was used most often (39%), followed by the American Dental Association tool13 (22%), California Dental Association tool9 (22%), and other forms or templates (17%). With at-risk patients, clinicians most often recommended fluoride toothpaste, setting a frequent recare interval, and providing oral health instruction as primary means of guiding care. Although prescription fluoride gel and paste have been shown to promote remineralization and oral health,45 fewer than 50% of study participants recommended prescription fluoride agents.2
Two analyses (of adults and children) completed by members of the Dental Practice-Based Research Network specifically evaluated dentists’ use of CRA tools.3,46 The adult analysis demonstrated that 69% of responding dentists (n=547) assessed risk by some methodology, with 17% using an established form.3 Public health and large group practices were most often associated with CRA use. In addition, 83% of respondents who graduated in the last 10 years reported using CRA, compared to 60% of dentists with 30 or more years of experience. In the pediatric analysis (ages 6 to 18), 73% of respondents (n=509) reported performing CRA, with 14% assessing risk using an established form.46 Among practitioners, care teams at large group practices were the most likely to administer CRA, as were recent dental school graduates. Trueblood et al47 report that 38% of Texas pediatric dentists (n=127) performed CRA on more than 75% of their patients. The study also showed that 40% admitted to not documenting risk status, and 9% did not assess risk.
WORKFLOW IMPLEMENTATION
The implementation of risk assessment processes in dental practice is varied, and most often reflective of business models, practitioner education and training, and the patient population being served. As these processes add elements to the visit that focus on patient behavioral changes, they can be challenging to integrate into patient care. There are distinct components, however, that can be sequenced and used as a guide during implementation. Figure 3 provides a workflow diagram representing how clinicians can incorporate CRA into the patient visit.48 After engaging the patient, care teams should use an established form to document the patient’s risk and protective factors. In addition, MI techniques can be used to gain buy-in and provide a better understanding of what is most important to the patient.37–40

Following the intraoral, head and neck examination, risk status and the course of treatment should be verified and discussed with the patient. The practitioner can engage the patient to help set realistic and specific self-management goals the patient can work on at home. Self-management goals should be tailored to fit patient characteristics. Individuals with numerous risk factors, for example, tend to benefit from setting of a finite number of goals (say, one to three), rather than trying to address all risk factors at once.49 Documentation of the patient’s self-management goals is needed to allow appropriate follow-up at recare appointments. When properly performed, risk assessment should be a conversation that ultimately leads to behavior change and improved oral health.
CONCLUSION
Implementing risk assessment can pose challenges to established practices, but it is instrumental in changing patient behavior and understanding patients. Risk assessment provides a framework that educates and motivates patients toward better health. It is not enough to simply assess risk for disease; rather, risk assessment guides action that will decrease the impact of risk factors and increase protective factors. True risk-based treatment planning allows medical and dental teams to provide timely care to patients at highest risk, while also helping to prevent future disease. Surely, the reliability and validity of risk assessment tools will continue to evolve, and clinicians who embrace risk-based care will provide the evidence that drives the future of dental practice.
REFERENCES
- American Academy of Family Physicians. High Impact Changes for Practice Transformation. Available at: aafp.org/practice-management/ transformation/pcmh/high-impact.html. Accessed January 18, 2017.
- Francisco EM, Johnson TL, Freudenthal JJ, Louis G. Dental hygienists’ knowledge, attitudes and practice behaviors regarding caries risk assessment and management. J Dent Hyg. 2013;87:353–361.
- Riley JL, Gordan VV, Ajmo CT, Bockman H, Jackson MB, Gilbert GH. Dentists’ use of caries risk assessment and individualized caries prevention for their adult patients: findings from the Dental Practice Based Research Network. Community Dent Oral Epidemiol. 2011;39:564–573.
- Reich E, Lussi A, Newbrun E. Caries risk assessment. Int Dent J. 1999;49:15–26.
- Fontana M, Zero DT. Assessing patients’ caries risk. J Am Dent Assoc. 2006;137:1231–1239.
- Zero D, Fontana M, Lennon AM. Clinical applications and outcomes of using indicators of risk in caries management. J Dent Educ. 2001;65:1126–1132.
- Jenson L, Budenz AW, Featherstone JD, Ramos-Gomez FJ, Spolsky VW, Young DA. Clinical protocols for caries management by risk assessment. J Calif Dent Assoc. 2007;35:714–723.
- Featherstone JD. The caries balance: contributing factors and early detection. J Calif Dent Assoc. 2003;31:129–133.
- Featherstone JD, Domejean-Orliaguet SO, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35:703–713.
- Young DA, Featherstone JD. Caries management by risk assessment. Community Dent Oral Epidemiol. 2013;41:e53–e63.
- Bader JD, Shugars DA, Kennedy JE, Hayden WJ, Baker S. A pilot study of risk-based prevention in private practice. J Am Dent Assoc. 2003;134:1195–1202.
- American Academy of Pediatric Dentistry. Policy on use of caries-risk assessment tool (CAT) for infants, children and adolescents. Pediatr Dent. 2007;29:29–33.
- American Dental Association Caries Risk Assessment Forms. Available at: ada.org/~/media/ADA/Science%20and%20Re search/Files/topic_caries_over6.ashx. Accessed January 18, 2017.
- Bratthal D, Hansel Peterson G. Cariogram. A multifactorial risk assessment model for a multifactorial disease. Community Dent Oral Epidemiol. 2005;33:256–264.
- American Academy of Pediatrics. Oral Health Risk Assessment Tool. Available at: www2.aap.org/oralhealth/docs/riskassessme nttool.pdf. Accessed January 18, 2017.
- Tellez M, Gomez J, Pretty I, Ellwood R, Ismail AI. Evidence on existing caries risk assessment systems: are they predictive of future caries? Community Dent Oral Epidemiol. 2013;41:67–78.
- Lang NP, Suvan JE, Tonetti MS. Risk factor assessment tools for the prevention of periodontitis progression: a systematic review. J Clin Periodontol. 2012;42(Suppl 16):S59–S70.
- Lang NP, Tonetti MS. Periodontal diagnosis in treated periodontitis. Why, when and how to use clinical parameters. J Clin Periodontol. 1996;23:240–250.
- Page RC, Martin J, Krall EA, Mancl L, Garcia R. Longitudinal validation of a risk calculator for periodontal disease. J Clin Periodontol. 2003;30:819–827.
- Papapanou PN. Periodontal diseases: epidemiology. Ann Periodontol. 1996;1:1–36.
- Tonetti MS. Cigarette smoking and periodontal diseases: etiology and management of disease. Ann Periodontol. 1998;3:88–101.
- Zohra L, Krishnan P, Mishra A, Reddy K. Evaluation and comparison of periodontal risk with three different risk assessment models — A cross sectional study. J Applied Dent Med Sci. 2016;2:3–9.
- Chandra RV. Evaluation of a novel periodontal risk assessment model in patients presenting for dental care. Oral Health Prev Dent. 2007;5:39–48.
- Lang NP, Tonetti MS. Periodontal risk assessment (PRA) for patients in supportive periodontal therapy (SPT). Oral Health Prev Dent. 2003;1:7–16.
- Lindskog S, Blomlof J, Persson I, et al. Validation of an algorithm for chronic periodontitis risk assessment and prognostication: risk predictors, explanatory values, measures of quality, and clinical use. J Periodontol. 2010;81:584–593.
- Teich ST. Risk assessment-based individualized treatment (RABIT): a comprehensive approach to dental patient recall. J Dent Edu. 2013;77:448–457.
- Busby M, Chapple E, Matthews R, Chapple IL. Practitioner evaluation of a novel online integrated oral health and risk assessment tool: a practice pilot. Br Dent J. 2013;215:115–120.
- Casamassimo P, Silverman J. Considerations for caries-risk assessment in an essential health benefits dental plan for children. American Academy of Pediatric Dentistry, Pediatric Oral Health Research and Policy Center Technical Report. 2012:1–2012.
- McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff. 2002;21:78–93.
- Booske BC, Athens JK, Kindig DA, Park H, Remington PL. Different perspectives for assigning weights to determinants of health. Available at: uwphi.pophealth.wisc.edu/ publications/other/different-perspectives-forassigning- weights-to-determinants-ofhealth. pdf. Accessed January 18, 2017.
- U.S. Department of Health and Human Services. Ten Leading Causes of Death in the United States. Available at: stacks.cdc.gov/ view/cdc/7655. Accessed January 18, 2017.
- McGovern L, Miller G, Hughes-Cromwick P. The Relative Contribution of Multiple Determinants to Health Outcomes. Available at: http://healthaffairs.org/healthpolicybriefs/ brief_pdfs/healthpolicybrief_123.pdf. Accessed January 18, 2017.
- Newton TJ, Asimakopoulou K. Managing oral hygiene as a risk factor for periodontal disease: a systematic review of psychological approaches to behavior change for improved plaque control in periodontal management. J Clin Periodontol. 2015;42(Suppl 16):S36–S46.
- Michie S, van Stralen M, West R. The behavior change wheel: a new method for characterizing and designing behavior change interventions. Implement Sci. 2011;6:42–49.
- Martins RK, McNeil DW. Review of motivational interviewing in promoting health behaviors. Clin Psychol Rev. 2009;29:283–293.
- Harrison R, Benton T, Everson-Stewart S, Weinstein P. Effect of motivational interviewing on rates of early childhood caries: a randomized trial. Pediatr Dent. 2007;29:16–22.
- Kay EJ, Vascott D, Hocking A, Nield H. Motivational interviewing in general dental practice: a review of the evidence. Br Dent J. 2016;221:785–791.
- Bray KK, Catley D, Voelker MA, Liston R, Williams KB. Motivational interviewing in dental hygiene education: curriculum modification and evaluation. J Dent Edu. 2013;77:1662–1669.
- Ramos-Gomez FJ, Crystal YO, Ng MW, Crall JJ, Featherstone JD. Pediatric dental care: prevention and management protocols based on caries risk assessment. J Calif Dent Assoc. 2010;38:746–761.
- Williams KB, Kimberly Bray RD. Motivational Interviewing: A Patient-centered Approach to Elicit Positive Behavior Change. Available at: dentalcare.com/en-us. Accessed January 18, 2017.
- Kay E, Vascott D, Hocking A, Nield H, Dorr C, Barrett H. A review of approaches for dental practice teams for promoting oral health. Community Dent Oral Epidemiol. 2016;44:313–330.
- Jonsson B, Ohrm K, Oscarson N, Lindberg P. The effectiveness of an individually tailored oral health education programme on oral hygiene behavior in patients with periodontal disease: a blinded randomized controlled clinical trial (one year follow up). J Clin Periodontol. 2009;36:1025–1034.
- Munster Halwarin AE. Self-determined motivational predictors of increases in dental behaviours, decreases in dental plaque, and improvement in oral health. A randomized clinical trial. Health Psychol. 2012;31:777–788.
- Kakudate N, Morita M, Sugai M, Kawanami M. Systematic cognitive behavioral approach for oral hygiene instruction. A short term study. Patient Ed Couns. 2009;74:191–196.
- Castellano JB, Donly KJ. Potential remineralization for demineralized enamel after application of fluoride varnish. Am J Dent. 2004;17:462–464.
- Riley JL III, Qvist V, Fellows JL, et al. Dentists’ use of caries risk assessment in children: findings from the Dental Practice- Based Research Network. Gen Dent. 2010;58:230–234.
- Trueblood R, Kerins CA, Seale SN. Caries risk assessment practices among Texas pediatric dentists. Pediatr Dent. 2008;30:49–53.
- DentaQuest Institute Caries Risk Assessment Workflow checklist. Available at: files.constantcontact.com/99f50496001/79021 4fe-09e1-4478-a511- 6f4f91a3b150.pdf?ver=1478623425000. Accessed January 18, 2017.
- Dalton AN, Spiller SA. Too much of a good thing: The benefits of implementation intentions depend on the number of goals. J Consumer Res. 2012;39:600–614.
Featured photo by BRIANAJACKSON/GETTY IMAGES
From Decisions in Dentistry. February 2017;3(2):53–57.





