Managing Cavitated Lesions in Patients Who Abuse Methamphetamine
An exploration of the effects of the nonmedical use of this drug on hard and soft oral tissues, as well as suggested clinical interventions.
PURCHASE COURSE
This course was published in the November 2016 issue and expires 11/30/19. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Discuss the increase in methamphetamine abuse and prevalence of oral health issues as a comorbidity in long-term users.
- Describe the potential oral manifestations of methamphetamine use.
- List therapeutic approaches to address the oral health consequences of nonmedical use of the drug.
- Explain the physiological effects of this stimulant, and the appropriate response when patients present with signs of use.
In a 2008 study, the United Nations Office on Drugs and Crime estimated there were 25 million users of methamphetamine globally.1 Between 2008 and 2014, however, the number of methamphetamine abusers more than doubled. Worldwide, as many as 52 million people between the ages of 15 and 64 are estimated to have used amphetamine-type stimulants for nonmedical purposes in 2014.2 It is the second most widely abused recreational drug (following cannabis).2 Methamphetamine can be snorted, smoked, ingested, injected and inserted rectally.3 It exerts a powerful effect through its activation of the dopamine, norepinephrine and serotonin systems. Its highly addictive properties are associated with the drug’s prolonged half-life (10 to 12 hours) and long duration of action, as well as its elevation of dopamine levels.2
A group heavily impacted by methamphetamine use is men who have sex with men; however, methamphetamine seems to appeal equally to men and women.4 Research indicates that women are more likely than men to use methamphetamine for weight loss and to relieve symptoms of depression.4 A 2010 study by Shetty et al5 on the dental effects of methamphetamine use reported dental disease — at 41.3% — as one of the most prevalent comorbidities in long-term methamphetamine users. A more recent investigation by Shetty et al6 notes that cigarette smokers who abuse methamphetamine were nearly three times as likely as nonsmokers to have untreated caries, and that, overall, posterior teeth (especially occlusal surfaces) were most affected. The researchers suggest the patterns of root caries in methamphetamine users are distinct and potentially could be used for identifying covert drug users. In addition, they report that while 37% of adults ages 35 to 49 in the U.S. general population have total periodontitis, more than 89% of methamphetamine users present with total periodontitis.
Another study demonstrated that chronic methamphetamine use has strong potential to damage the stomatognathic system. The direct consequence of abuse — including xerostomia, bruxism, decreased salivary buffering capacity, and accompanying risk factors, such as consumption of other toxic substances — may contribute to an overall neglect of dental care, significantly increasing oral health risks7 (Figures 1A through 3B).

show the early stages of oral decay in a methamphetamine user: (A) caries and demineralization, starting at the gingival margins and progressing to the entire buccal or labial surface, including occlusal caries in posterior teeth; and (B) gingivitis with accompanying xerostomia. Photos Courtesy of MITCHELL GOODIS, DDS


the advanced stages of methamphetamine
abuse include: (A) teeth broken off at the gingival margin; and (B) grayish-brown dentition with enamel that is reduced to a soft, leathery texture, along with gingivitis and acute periodontitis.
PATIENT MANAGEMENT
Tatlock et al8 suggest the following protocol when treating patients with methamphetamine-induced oral conditions:
- Include questions about drug use when taking a medical history
- Consider the potential for drug interactions to rule out possible contraindications
- Be aware that administering nitrous oxide or prescribing narcotics could endanger a recovering patient’s sobriety • Offer education about regular checkups and oral hygiene (e.g., flossing and brushing with a fluoride toothpaste for two minutes at least twice daily)
- Suggest a mouthguard for patients who brux
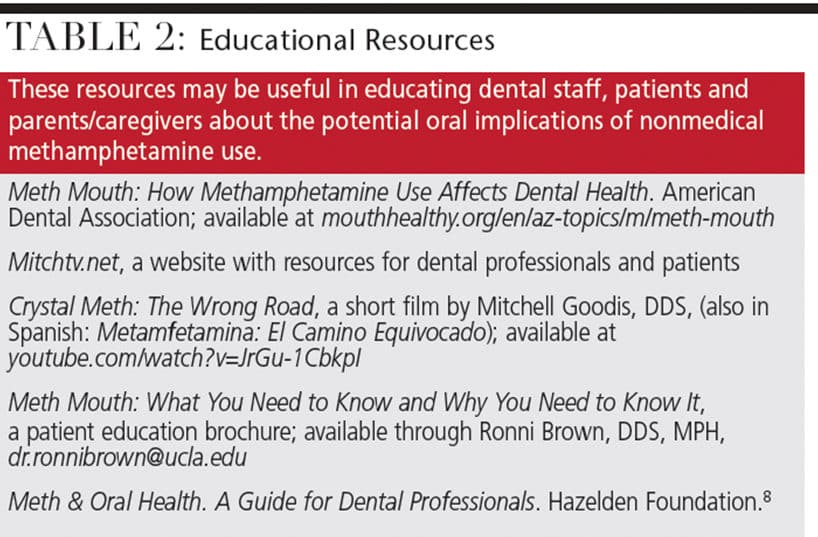
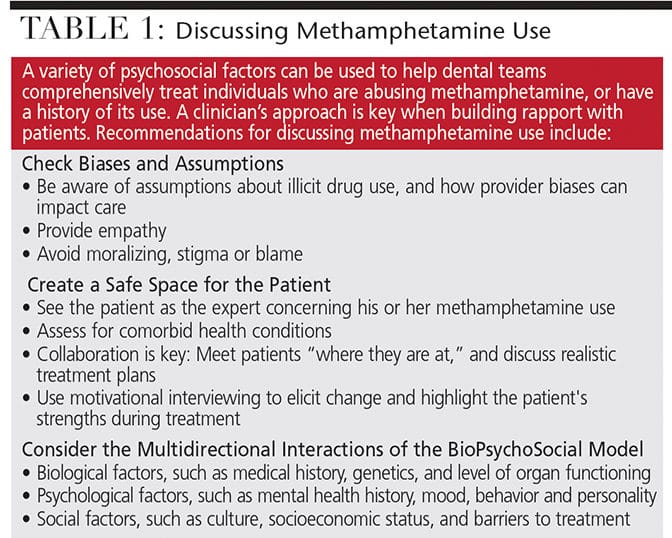
Discussions with patients about the oral health risks associated with nonmedical amphetamine use should be tactful and nonjudgmental (Table 1). In addition, patient education efforts should explain the benefits of a balanced diet and drinking water rather than sugary beverages or diuretics (such as caffeine and alcohol) that can exacerbate xerostomia. Table 2 (page 40) offers a sampling of methamphetamine educational resources.
 It is difficult, if not impossible, to mitigate the oral effects of methamphetamine if substance abuse is ongoing. For patients in all stages of methamphetamine use, clinicians should explain optimal short-term and long-term treatment options. Patients are often embarrassed by their teeth and appreciate guidance for esthetic and functional improvements. Treatment of cavitated lesions using glass ionomer as an interim restoration — with or without removal of decay — can slow or possibly stop lesion progression. Stabilizing lesions in this manner can help see the patient through a drug addiction rehabilitation period with reasonable esthetic and functional improvement.
It is difficult, if not impossible, to mitigate the oral effects of methamphetamine if substance abuse is ongoing. For patients in all stages of methamphetamine use, clinicians should explain optimal short-term and long-term treatment options. Patients are often embarrassed by their teeth and appreciate guidance for esthetic and functional improvements. Treatment of cavitated lesions using glass ionomer as an interim restoration — with or without removal of decay — can slow or possibly stop lesion progression. Stabilizing lesions in this manner can help see the patient through a drug addiction rehabilitation period with reasonable esthetic and functional improvement.
If a patient is in recovery, or has expressed a desire to save his or her teeth, the authors present the following method for caries management using silver diamine fluoride (SDF). In 2014, the U.S. Food and Drug Administration cleared SDF for marketing as a dental desensitizing agent, and many state regulatory boards have approved its application by dental auxiliaries. This agent has been used off-label to arrest caries, primarily in high-risk caries patients. Although such use has been shown to be effective and safe,9,10 as with all off-label therapy, clinicians are advised to exercise professional judgment.
Methamphetamine users suffer rampant decay for a variety of reasons. The drug contributes to xerostomia, and, among this patient population, oral health is further compromised by the tendency to neglect proper nutrition, oral hygiene and regular dental visits.7,8 Individuals subject to drug addiction often do not have the financial resources for extensive dental reconstruction. In these cases, SDF offers a potential first step for oral rehabilitation by stabilizing the progression of caries lesions until recovery and rehabilitation can begin.
The first step in treatment is to engage the patient and obtain consent with the understanding that SDF is not definitive care, but, rather, the beginning of care. Clinicians should also explain that SDF will darken cavitated surfaces (Figure 4).11 Improvement in the appearance of teeth can begin when decay is arrested and the patient is ready to move forward and participate actively in recovery, leading to improved oral health. If resources are available, esthetic concerns can be addressed with conventional dental services (e.g., direct or indirect restorations, and fixed or removable prostheses).
Teeth to be treated must be free of symptoms of pulpitis, signs of draining fistula or pulpal exposure. One to two drops of SDF are dispensed into a plastic dappen dish. The affected dentition is polished with prophylaxis paste, or thoroughly cleaned with a toothbrush. The teeth are then isolated with cotton rolls and dried. Using a microbrush, the solution is applied to the affected area for one minute, and the excess is rinsed off. Most patients report a metallic or bitter taste during treatment, but there is no other discomfort.11 Patients are instructed not to eat, drink or brush for one hour following treatment.
For severe caries, some protocols recommend reapplication of SDF after two, four, six and eight weeks.12 Although other protocols recommend fewer initial treatments,11 consensus is that treatment should continue until lesions are arrested (or restored), and repeated biannually or annually to maintain the result.
Care must be used in handling SDF because it will stain surfaces; consequently, plastic wrap or other barrier products are recommended to protect operatory surfaces. This agent should not be splashed onto clothing or skin. If it contacts skin, SDF will leave a dark stain, which will exfoliate in one to two weeks.9
REMINERALIZATION AND REFERRAL
Because methamphetamine users are subject to high caries risk, remineralization therapies are often indicated to prevent the development of new lesions or progression of existing decay. Thus, concentrated fluoride products may be prescribed as part of the treatment plan. Clinicians can refer to the caries management by risk assessment — or CAMBRA — protocol for further information about caries management strategies.13
As noted, clinicians should be mindful that it is difficult to mitigate oral health problems if methamphetamine use is ongoing. If a patient is abusing methamphetamine, referral to a substance abuse treatment center should be offered,8,14 and dental offices should maintain a list of local and national resources for this purpose. It is recommended that the office have written information available detailing addiction support services.14

Whenever possible, dental teams should coordinate with the patient’s physician so that he or she may participate in the referral. If the patient does not wish to discuss illicit drug use with oral care professionals, the team should document findings in an objective, nonjudgmental manner. The patient should also be encouraged to return to the practice for follow-up care.
TREATMENT PRECAUTIONS
For the safety of patients and staff, all team members should be able to identify the signs of an intoxicated methamphetamine user. When taking the drug, users report feelings of euphoria, an abundance of energy, increased motivation, anxiety, increased self-confidence and decreased appetite. Physiological effects include elevated heart rate, increased blood pressure, hypertension, hyperthermia, pupil dilatation, sweating, insomnia, dermatologic reactions and psychomotor agitation.4,15,16 It is not unusual for individuals who abuse methamphetamine to engage in binge episodes in which they use large amounts of the drug for several days, and neglect proper dietary, hygienic and personal care.
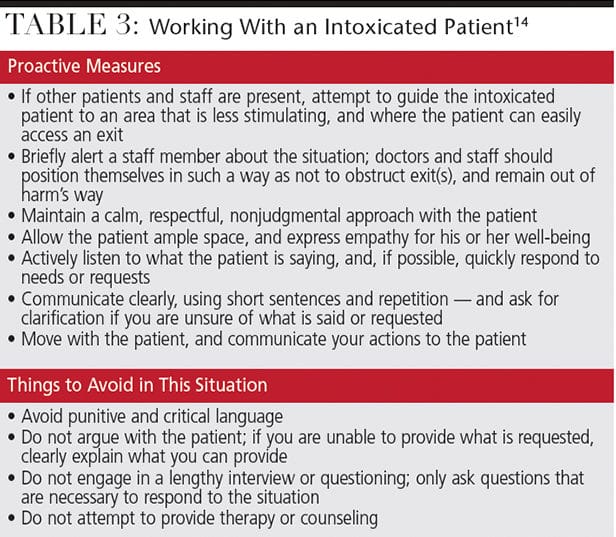
If the clinician suspects that a patient is intoxicated due to signs of recent use — such as repetitive physical activity, rapid speech, shortness of breath, irritability or bruxing — dental treatment should not be administered for physiological reasons.14 Furthermore, due to the patient’s mental functioning, he or she may not be able to make informed decisions regarding treatment or consent. In these situations, the clinician should inform the patient in a calm and clear manner that, for safety reasons, the team will not be able to provide treatment at this time. Table 3 provides guidelines and precautions for working with intoxicated patients.14
 CONCLUSION
CONCLUSION
Drug addiction has severe psychosocial and physical consequences, and this is especially true with methamphetamine users, who are subject to a variety of oral health issues. Through therapeutic interventions, including glass ionomer, SDF and concentrated fluoride — and by offering patient education and referral to substance abuse resources — dental professionals can help recovering users reintegrate into mainstream society by restoring teeth and smiles.
REFERENCES
- United Nation Office on Drugs and Crime. Annual Report 2008. Available at: unodc.org/documents/about-unodc/AR08_WEB.pdf. Accessed October 5, 2016.
- Radfar SR, Rawson RA. Current research on methamphetamine: Epidemiology, medical and psychiatric effects, treatment, and harm reduction efforts. Addict Health. 2014;6:146–154.
- Shrem MT, Halkitis PN. Methamphetamine abuse in the United States: contextual, psychological and sociological considerations. J Health Psych. 2008;13:669–679.
- Gonzales R, Mooney L, Rawson RA. The methamphetamine problem in the United States. Annu Rev Public Health. 2010:31:385–398.
- Shetty V, Mooney LJ, Zigler CM, Belin TR, Murphy D, Rawson R. The relationship between methamphetamine use and increased dental disease. J Am Dent Assoc. 2010;141:307–318.
- Shetty V, Harrell L, Murphy DA, et al. Dental disease patterns in methamphetamine users: Findings in a large urban sample. J Am Dent Assoc. 2015;146:875–885.
- Rommel N, Rohleder NH, Wagenpfeil S, et al. The impact of the new scene drug “crystal meth” on oral health: a case-control study. Clin Oral Invest. 2016;20:469–475.
- Tatlock C, Wagner S, Williams N. Meth & Oral Health. A Guide for Dental Professionals. Available at: www.securiandental.com/cm_files/pdf/ 050208_SecurianMethBookletFinal.pdf. Accessed October 5, 2016.
- Featherstone JD, Horst JA. Fresh approach to caries arrest in adults. Decisions in Dentistry. 2015;1(1):36–44.
- Horst JA, Ellenikiotis H, Milgrom PM. UCSF protocol for caries arrest using silver diamine fluoride: rationale, indications, and consent. J Calif Dent Assoc. 2016;44:16–28.
- Fa BA, Horst JA, Hirsch JP, Duffin S, Wong A, Young DA. Caries arrest with silver diamine fluoride. Decisions in Dentistry. 2016;2(10):48–51.
- Duffin S. Back to the future: the medical management of caries introduction. J Calif Dent Assoc. 2012;40:852–858.
- Featherstone JD. The caries balance: contributing factors and early detection. J Calif Dent Assoc. 2003;31:129–133.
- Jenner L, Lee N. Treatment Approaches for Users of Methamphetamine: A Practical Guide for Frontline Workers. Available at: nationaldrugstrategy.gov.au/ internet/drugstrategy/publishing.nsf/Content/8D2E281FAC2346BBCA25764D007D2 D3A/$File/tremeth.pdf. Accessed October 5, 2016.
- Rusyniak DE. Neurologic manifestations of chronic methamphetamine abuse. Psychiatr Clin North Am. 2013;36:261–275.
- Cruickshank CC, Dyer KR. A review of the clinical pharmacology of methamphetamine. Addiction. 2009;104:1085–1099.
Feature Photo Courtesy of KAARSTEN/ISTOCK/ THINKSTOCK
From Decisions in Dentistry. November 2016; 2(11): 36, 39-41.