
Digital Workflow for Implant Dentistry
Implementing advanced technologies aids in diagnosis, treatment planning and delivery of dental implant therapy.
There are several stages of technology and innovation adoption that have been quantified and categorized across industries. In recent years, digital dentistry has evolved beyond the innovator and early adopter stage, which was characterized by a small group that represents only 16% of the dental profession.1 These visionaries had the foresight and knowledge needed to implement the technology before it was efficient, intuitive and mainstream — setting the stage for later adopters.
Today, digital dental technology is entering into the mainstream stage and is used by approximately 34% of clinicians.1 This is perhaps the most exciting phase in the evolution of technology adoption. The community of users is growing at a fast rate, leading to advances and innovations in multiple platforms that can be synergistically combined to improve outcomes.
Implant procedures are one of the most exciting facets of dentistry that has been enhanced by digital technology. The innovations explored in this discussion provide clinicians with the tools for diagnosis, planning, placement and restoration of implants in a truly transformative way — one that is quickly becoming the standard of care.
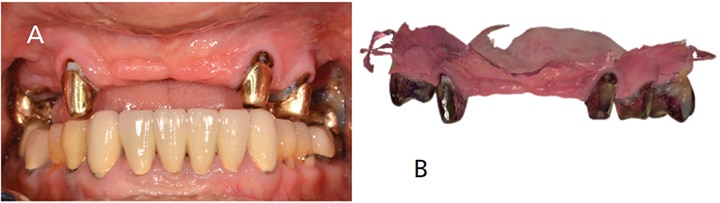
DIGITAL DIAGNOSTIC IMPRESSIONS
Intraoral digital impressions of the presurgical area are a critical first step in the digital workflow (Figures 1A and 1B, and Figures 2A through 2D). Although evidence in the literature is mixed regarding the accuracy and practicality of complete arch digital impressions, the current generation of digital impression systems is more accurate for full arches and faster than previous systems.2 Furthermore, digital models generated by these modalities have been shown to be as reliable as plaster cast models.3 These traits depend on the accuracy of the scanner and mathematical algorithm used to construct the digital model from individual images. Current scanners have been shown to be quite accurate, with an accuracy range of 6.9 µm to 45.2 µm.4 These scanners also acquire and render three-dimensional (3D) models easily and rapidly, which has led to growing use by clinicians and increased preference by patients.5

situation is merged with the intraoral scan of the patient’s teeth and gingiva,
allowing for visualization that aids in diagnosis and treatment planning.
DIAGNOSTIC WAX-UP
The diagnostic wax-up is a critical component in implant treatment planning. In specialized laboratory or chairside software, the intraoral scan is merged with facial photos, allowing for a patient-specific digital wax-up and rapid prototyping of smiles without the patient being present (Figures 3A and 3B, and Figure 4). Multiple tooth shapes and sizes can be selected and the software lets clinicians and technicians visualize how the virtual wax-up will appear in the smile (Figure 4). This allows for prosthetically driven implant planning. When the wax-up is finalized, the patient can visualize the case prior to treatment, and adjustments can be made to tooth shape, size or morphology. Once the final design is complete, the digital wax-up can be produced via 3D printing or milling and tried in the patient’s mouth (Figure 5).

tooth molds to allow patients to choose which option is most pleasing to them.
CONE BEAM COMPUTED TOMOGRAPHY
Conventional radiographs suffer from the same two-dimensional limitations of the original radiograph developed in the 19th century by Wilhelm Roentgen.6 In the 1970s, however, Sir Godfrey Newbold Hounsfield discovered that radiographs taken from multiple angles could be reconstructed into a 3D image.7 As computer processing power expanded, the technology has developed to the point where clinicians can now rapidly scan and, in near instant time, produce an ultra-high-resolution 3D rendering of the patient’s oral anatomy. With low-dosage optimization bringing cone beam computed tomography (CBCT) radiation in line with conventional panographs, CBCT has become the standard of care for implant placement.8–11 Compared to medical-grade computed tomography, dental CBCT scans have the capacity to capture 3D structures with short scan times and ultra-low dosages.8 The accuracy of the data acquired by these scans has been verified in the literature, as has its ability to help clinicians assess and quantify the bone for future implant sites.9,10 In comparison to direct measurements, Timock et al11 demonstrated its ability to discriminate alveolar bone thicknesses between 0.13 to 0.3 mm, and without discernable over or underestimation.


IMPLANT PLANNING SOFTWARE
In 1988, a breakthrough concept was introduced: dental software that reformatted CBCT images in a way that was useful for diagnosis and treatment planning. The software continued to evolve and, in 1993, software was introduced that allowed clinicians to overlay virtual implants on cross-sectional images for verification of proper planning. Although useful, no real translation of the virtual surgical plan to the patient was possible until technology was introduced in 2002 for drilling osteotomies to an exact location, angulation and depth using the virtual plan.12

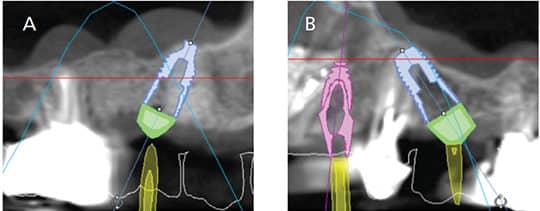
Now, in addition to allowing practitioners to accurately assess bone volume, bone density and restorative space, the location of the prosthesis can be merged from the digital wax-up and preoperative scan for prosthetically driven implant planning (Figure 6A through Figure 9). Furthermore, critical anatomic landmarks — such as nerves, sinuses and proximal teeth — can be identified and avoided through safety zones in the planning software (Figure 7). In summary, the software allows for accurate determinations of implant width, depth and size prior to surgery; it also helps clinicians visualize the prosthetic plan to aid in presurgical planning. When planning multiple implants, each can be instantly paralleled using the software, which greatly simplifies restoration of complicated cases (Figure 9).

COMPUTER-GUIDED SURGERY
These virtually placed implants have been carefully planned using all the necessary merged information to ensure they are at the ideal angulation, location and depth to support optimal prosthetic results. On the day of surgery, this planning is “transferred” to the patient via the surgical guide, which is made with either an additive steriolithographic 3D printing process or a subtractive milling process. Some software platforms allow in-office 3D printing or milling of surgical guides, while others require off-site fabrication.

Once fabricated, the benefits to the clinician and patient are significant. Compared to freehand surgery, it has been shown that using a computer-generated surgical template significantly reduces the chance for a positional error at the time of implant placement.13 Arisan et al14 reported a 6% probability of a positional error using a computer guided template, and an 88% probability of having a positional error with a freehand approach. These benefits combine to allow greater precision in implant placement and increased restorative simplicity.15
The benefits of guided surgery are not limited to those affecting the dental provider. Patients benefit by experiencing significantly less intraoperative and postoperative complications, including pain.16 Increased patient comfort has been linked to the benefit of not having to raise a flap for surgery and has been shown to be the preferable method for executing guided surgery.17,18 In addition to preserving periostium contact with bone, blood supply and osteogenic potential, Cosyn et al19 demonstrated that the flapless technique enhanced esthetics by preserving papilla.
NAVIGATION (ROBOTIC) SURGERY
An emerging approach to implant placement is the use of navigation, also termed robotic surgery. This involves the use of tracking devices attached to the patient and implant handpiece. These two positions in space are relayed to a central processing unit and superimposed on a monitor. Their relation to the previously planned implant osteotomy is displayed, and the implant handpiece can be adjusted by following the onscreen graphics. This technology eliminates the need for a surgical template, as used in computer-guided surgery, and allows real-time correction of the osteotomy during the procedure.
SCAN BODIES
Digital impressions can also be applied in the restorative phase of implant dentistry. Intraoral scan bodies have been developed for most major implant brands, which allows the use of the majority of intraoral scanning devices on the market. These scan bodies allow for the implant brand, position and timing to be registered and transferred to a digital model. All of the necessary information relative to provisional treatment, opposing arch, and bite registrations can be captured with intraoral scanners. This workflow has proven to be efficient and accurate for dentate and edentulous cases.20 Patients and clinicians benefit from quicker treatment times with digital techniques;21 furthermore, patients in one study unanimously preferred digital impressions over conventional impressions.22
ABUTMENTS AND RESTORATION
These digital impressions can be sent to a laboratory through a Health Insurance Portability and Accountability Act-compliant network, or remain in the scanning system for in-office fabrication of the final abutment and prosthetic. In complicated cases, most clinicians will find it useful to work with a dental laboratory. The dental technician has the ability to use sophisticated technology to design and manufacture the corresponding restorative components. Digital laboratory technologies reduce the number of error-inducing steps and manipulations of materials, and thus have been associated with more efficient processes.23 Custom abutments are designed digitally and milled out of the material of the clinician’s choice.
These digital design and manufacturing methods have gained popularity due to their ability to simplify and streamline the complex process of fabricating restorations.24 Digitally designed and milled provisional restorations can be fabricated before the surgical procedure for immediate temporization. When comparing this digital workflow to a conventional approach, digital technology has been shown to be three times more efficient for the formation of implant-supported crowns. This workflow also benefits the clinician, as the mean clinical adjustment and seating time is significantly faster than for restorations fabricated with conventional methods.25
KEY TAKEAWAYS
- Advances in digital technologies provide clinicians with the tools for diagnosis, treatment planning, placement and restoration of implants in a truly transformative way.
- Digital dental technology is entering into the mainstream stage of adoption, and is used by approximately 34% of clinicians.1
- Intraoral digital impressions of the presurgical area are a critical first step in the digital workflow.
- With low-dosage optimization bringing cone beam computed tomography (CBCT) radiation in line with conventional panographs, CBCT has become the standard of care for implant placement.8–11
- Besides allowing practitioners to accurately assess bone volume, bone density and restorative space, the location of the prosthesis can be merged from the digital wax-up and preoperative scan for prosthetically driven implant planning.
- Furthermore, critical anatomic landmarks — such as nerves, sinuses and proximal teeth — can be identified and avoided through safety zones in the planning software.
- Compared to freehanded surgery, using a computergenerated surgical template significantly reduces the chance for a positional error at the time of implant placement.13
- Digitally designed and milled provisional restorations can be fabricated before the surgical procedure for immediate temporization.
REFERENCES
- Rogers EM. Diffusion of Innovations. 5th ed. New York, NY: The Free Press; 2003:289–290.
- Renne W, Ludlow M, Fryml J, et al. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J Prosthet Dent. 2016;16:30514–30515.
- Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi C. Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review. Am J Orthod Dentofacial Orthop. 2016;149:161–170.
- Hack G, Patzelt S. Evaluation of the accuracy of six intra-oral scanning devices: An in-vitro investigation. J Am Dent Assoc. 2015;10;1–5.
- Schepke U, Meijer HJ, Kerdijk W, Cune MS. Digital versus analog complete-arch impressions for single-unit premolar implant crowns: Operating time and patient preference. J Prosthet Dent. 2015;114:403–406.
- Marsh H. A case of Roentgen photography. Br Med J. 1896;1:1318–1320.
- Hounsfield GN. Computed medical imaging. Science. 1980;210:22–28.
- EzEldeen M, Stratis A, Coucke W, Codari M, Politis C, Jacobs R. As low dose as sufficient quality: optimization of cone-beam computed tomographic scanning protocol for tooth autotransplantation planning and follow-up in children. J Endod. 2017;43:210–217.
- Agbaje JO, Jacobs R, Maes F, Michiels K, van Steenberghe D. Volumetric analysis of extraction sockets using cone beam computed tomography: a pilot study on ex vivo jaw bone. J Clin Periodontol. 2007;34:985–990.
- Lund H, Gröndahl K, Gröndahl HG. Accuracy and precision of linear measurements in cone beam tomography Accuitomo tomograms obtained with different reconstruction techniques. Dentomaxillofac Radiol. 2009;38:379–386.
- Timock AM, Cook V, McDonald T, et al. Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 2011;140:734–744.
- D’haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A. Current state of the art of computer-guided implant surgery. Periodontol 2000. 2017;73:121–133.
- Di Giacomo G, Cury PR, de Araujo NS, Sendyk WR, Sendyk CL. Clinical application of stereolithographic surgical guides for implant placement: preliminary results. J Periodontol. 2005;76:503–507.
- Arisan V, Karabuda CZ, Mumcu E, Özdemir T. Implant positioning errors in freehand and computer-aided placement methods: a single-blind clinical comparative study. Int J Oral Maxillofac Implants. 2013;28:190–204.
- Van Assche N, Vercruyssen M, Coucke W, Teugheis W, Jacobs R, Quirynen M. Accuracy of computer-aided implant placement. Clin Oral Implants Res. 2012;Suppl 6:112–123.
- Nkenke E, Eitner S, Radespiel-Tröger M, Vairaktaris E, Neukam FW, Fenner M. Patient-centred outcomes comparing transmucosal implant placement with an open approach in the maxilla: a prospective, non-randomized pilot study. Clin Oral Implants Res. 2007;18:809–814.
- Fortin T, Bosson JL, Isidori M, Blanchet E. Effecct of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants. 2006;21;298–304.
- Arisan V, Karabuda CZ, Ozdemir T. Implant surgery using bone-and mucosa-supported steriolithographic guides in totally edentulous jaws; surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Implants Res. 2010;21:980–988.
- Cosyn J, Hooghe N, De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol. 2012;39:582–589.
- Gherlone E, Cappare P, Vinci R, Ferrini F, Gastaldi G, Crespi R. Conventional versus digital impresions for “all-on-four” restorations. Int J Oral Maxillofac Implants. 2016;31:324–330.
- Joda T, Lenherr P, Dedem P, Kovaltschuk I, Bragger U, Zitzmann N. Time efficiency, difficulty, and operator’s preference comparing digital and conventional implant impressions: a randomized controlled trial. Clin Oral Impl Res. Sept. 5, 2016. Epub ahead of print.
- Joda T, Brägger U. Patient-centered outcomes comparing digital and conventional implant impression procedures: a randomized crossover trial. Clin Oral Implants Res. 2016;27:e185–e189.
- Abduo J, Bennamoun M, Tennant M, McGeachie J. Impact of digital prosthodontics planning on dental esthetics: Biometric analysis of esthetic parameters. J Prosthet Dent. 2016;115:57–64.
- Joda T, Brägger U. Complete digital workflow for the production of implant-supported single-unit monolithic crowns. Clin Oral Implants Res. 2014;25:1304–1306.
- Joda T, Katsoulis J, Brägger U. Clinical fitting and adjustment time for implant-supported crowns comparing digital and conventional workflows. Clin Implant Dent Relat Res. 2016;18:946–954.
The authors have no commercial conflicts of interest to disclose.
FEATURED IMAGE BY MEDIAPHOTOS/E+/GETTY IMAGES PLUS
From Decisions in Dentistry. July 2017;3(7):13—17.


