Dentists’ Evolving Role in Treating Cleft Lip and Palate
An overview of developments in care for this patient population, and the ever changing and expanding role of the dental provider.
This course was published in the November 2017 issue and expires November 2020. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
- Explain the prevalence of babies born with cleft lip and/or palate, and factors that play a role in its development.
- Discuss ways in which cleft lips and/or palates are detected, and the make-up of the interdisciplinary care team.
- List the goals of presurgical infant orthopedics, the ways in which nasoalveolar molding therapy addresses this condition, and the growing popularity of this treatment approach.
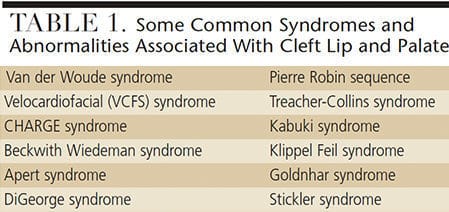
Clefts of the lip and/or palate affect children of all socioeconomic and cultural backgrounds, with an overall worldwide prevalence of approximately one in 700 live births.1 In the United States, it is estimated that nearly one in 1000 babies is born with an orofacial cleft.2 Interdisciplinary treatment is required, and this article will focus on developments in care, and the ever changing and expanding role of the dental provider. Clefts vary greatly in severity; one mild form, for example, is a submucous cleft, in which the soft palate is involved, but the oral tissues are intact. A submucous cleft may go undetected until toddler years, when abnormal speech may lead to a diagnosis. More severe clefts can involve the lip, hard palate, and, less frequently, facial structures. Clefts are classified as complete or incomplete, as well as unilateral or bilateral. Half of all orofacial clefts involve both the palate and lip, while clefts isolated to the palate are less common.2 This condition can result from isolated genetic mutations, environmental factors or teratogen exposures, including alcohol and tobacco. They are also associated with a number of syndromes (Table 1). While genetics may play a role in the development of orofacial clefts, both syndromic and nonsyndromic, genetics are not the sole determinant.
Caring for a child with cleft lip and/or palate (as well as caring for the family of the child) is an interdisciplinary task, one that starts even prior to birth. With advances in ultrasound technology, more orofacial clefts are being discovered in utero. While an exact percentage is difficult to determine, ultrasound detection rates of up to 75% have been reported,3 with the highest rates noted when three-dimensional and four-dimensional technologies are used.4 This is remarkable considering the first cleft deformity diagnosed by ultrasound technology was reported in 1981.5
INTERPROFESSIONAL CARE TEAM
As soon as a cleft lip or cleft palate is detected, the interdisciplinary cleft lip and palate team goes to work. The makeup of a cleft lip and palate team (sometimes referred to as a craniofacial team) differs depending on the institution, but typically consists of nursing, otolaryngology, plastic surgery, speech pathology, social work, audiology, orthodontics, oral surgery and pediatric dentistry professionals.
This interprofessional collaborative care model is a necessity because children with cleft lip and/or palate will often present with numerous health challenges, sometimes due to other components of a larger syndrome or condition. These challenges include, but are not limited to, middle ear abnormalities, frequent ear infections, hearing loss, and difficulty feeding due to clefting of the palate. A complete cleft of the palate may prevent breastfeeding and complicate bottle feeding. The simple task of getting adequate nutrition can be a major challenge for infants with clefts.
Traditionally, the role of an oral health professional on an interdisciplinary cleft lip and palate team has been to address the preventive and restorative needs of the child — much as with any other patient. In recent years, however, the oral health professional’s role has evolved with the rise of early orthopedic treatment of the predentate infant.
PRESURGICAL INFANT ORTHOPEDICS
The first member of the cleft lip and palate team to make contact with the family is often a nurse. This meeting will either take place during pregnancy, shortly after ultrasound reveals the cleft diagnosis, or at the time of birth, when a cleft is identified for the first time. The nurse will counsel the family on what to expect from their newborn and begin to lay the groundwork for future care. This can be an overwhelming time for parents and it takes a special individual to take on this counseling role. Nurses will discuss myriad issues with the family. One of these issues has dramatically altered the dentist’s role on the team: This is the topic of presurgical molding of the alveolus, also known as presurgical infant orthopedics (PSIO).
The idea behind PSIO is to normalize the anatomy of a cleft as much as possible prior to surgical repair; the overarching goals are to give the surgeon a better starting point, and make the surgical closure of the cleft defect less difficult. These can be achieved by bringing the bony alveolar segments into better alignment by applying forces to the oral tissues. This is not a new concept. The PSIO idea was born in 1950 when McNeil6 showed how orthodontic forces could be applied to a predentate infant to decrease the size of an alveolar cleft. This led to additional intraoral appliances that were based on this same concept. Subsequently, Latham et al7 developed an acrylic plate that applied forces to the maxillary arch to close a bony cleft, but this plate was inserted surgically and retained by a pin screwed into the infant’s hard palate. The “Latham appliance” is still used today, and movement is achieved by turning a screw — similar to one found on a rapid maxillary expansion device.

A simple version of PSIO is the use of elastomeric tape (Figure 1) across the maxillary lip8 to place a constrictive force on the palate. The tape has the benefit of being inexpensive and easy to use, but does not allow the provider to control the forces applied to the palate, so it will indiscriminately bring the tissues together — often leading to a constricted palate.
The most recent advance in this area is known as nasoalveolar molding (NAM). The NAM appliance (Figure 2) was pioneered by Grayson,9 and uses the same concept as McNeill’s acrylic plate, in which sequential changes to the internal surface of the plate bring the bony alveolar segments together. The main difference is that NAM incorporates a nasal stent that improves the cartilaginous architecture of the nose.

The primary advantage of NAM over elastomeric taping is that it does not result in constriction of the palate because the transverse dimension is held static by the custom-made acrylic plate. Compared to a Latham appliance, NAM’s primary advantage is that it does not require an additional surgery.
While the concept of molding the alveolus has been around for decades, the addition of the nasal stents separates NAM from other approaches. The idea for the stents came from research by Matsuo et al10 on the molding of infant’s ears to decrease deformity. The authors found that placing pressure on these deformed cartilaginous tissues resulted in visible and sustained improvement in the shape of the auricular tissues.

affected side.
Infants with complete clefts of the lip and palate often have associated nasal deformities. For babies with unilateral complete clefts, the affected side of the nose will have a flatter and more stretched nostril (Figure 3). A child with a complete bilateral cleft will often have very short columella (Figure 4). Grayson and Maull9 postulated that the same principles used on molding ear cartilage could improve the nasal shape of infants with clefts, thereby lessening the invasiveness of the surgical correction. Surgeons can use techniques to improve this nasal architecture, but any incision will result in scarring that has the potential to hinder future growth. Changes to these tissues that reduce the need for incisions and scarring are a major benefit of successful NAM treatment.

These advantages explain the popularity of PSIO. The dental provider — whether an orthodontist, pediatric dentist, or both working in concert — is on the front lines of caring for infants with a cleft lip and/or palate. The fabrication, adjustment and maintenance of NAM appliances dovetail with the skill set of dental professionals, particularly pediatric dentists and orthodontists.
NASOALVEOLAR MOLDING
The first step in the NAM process is to make an impression of the infant’s maxillary arch. This is done as soon as possible, as insertion of the NAM appliance at a very young age maximizes the malleability of the infant’s soft tissues. This increased ability to mold the infant’s tissues is thought to be due to an increase in maternal estrogen in the infant’s body,11 and is the same reason why auricular molding is more effective in young babies. The impression is made using a polyvinyl siloxane material that is not only dimensionally stable, but stays together well, thus reducing the risk for aspiration or swallowing. A member of the medical team is present chairside during the impression to provide support for any airway emergencies. Using this impression, a stone model of the palate is poured for the fabrication of an acrylic plate (Figure 5, Figure 6 and Figure 7) that fits the infant’s palate. With sequential internal modifications, this plate will be used to change the shape of the infant’s palate over the course of three to six months.
The NAM approach is neither a simple process nor a quick fix, as adjustments have to be made on a regular basis to continue the movement of the tissues. These adjustments alter the internal shape and thickness of the acrylic plate by approximately 1 mm, so the plate no longer fits ideally on the palate (Figure 8). As the appliance is worn and as the baby feeds with a bottle, pressure will begin to move and mold the tissues into the new shape. These adjustments are repeated on a weekly or biweekly (at minimum) basis over three to six months leading up to the initial surgical repair of the lip.

A chief goal of NAM is to decrease the size of the alveolar cleft as much as possible. Once the cleft is narrowed to 5 mm or less, the nasal stent can be added to the acrylic plate (Figure 9). A single nasal stent is used on the affected nostril for a child with a unilateral complete cleft, while two stents are used for a child with a bilateral complete cleft. The stent places pressure on the ala of the nose and to create a more natural convexity of both the alar rim and nasal dome. As these nasal cartilages are reshaped, a more symmetric appearance results and the tissues of the columella are straightened and lengthened, lessening the need for more invasive surgical techniques.12 The results of successful NAM treatment include closing of the bony alveolar cleft to within 5 mm, bringing the lip segments into closer proximity, elongating the columella, achieving convexity of the nasal cartilage, reducing the width of the nasal base, and achieving maximum symmetry of the nostrils.

Taking care of the NAM appliance and keeping it in place and functional can be challenging for families. The appliance is retained by tape attached to the child’s cheeks. Tape is integral to successful treatment because it not only provides force to activate the appliance, it also provides the upward force that keeps the appliance in contact with the palate. Improper taping can lead to a nonretentive appliance and frustrated caregiver. While it certainly can be challenging for families to use the NAM appliance (particularly at first), there is evidence that NAM therapy has psychosocial benefits for caregivers. A recent study examined caregivers from multiple U.S. cleft treatment centers;13 the subjects were divided up into groups, one of which had used NAM, and the other of which used traditional means of presurgical cleft care. Compared to the traditional treatment group, the NAM families had lower anxiety scores and a greater sense of empowerment. It was postulated the NAM group benefited from the regular weekly visits and support that they were able to receive as a result of these frequent trips.
The clinical benefits of the NAM appliance are still controversial. Many cleft lip and palate teams have established protocols (with predicable outcomes) utilizing Latham appliances, elastomeric taping or other methods, and may be reluctant to change. With NAM being a relatively new treatment modality, long-term data is minimal. While there may never be a consensus, a 2008 study found that more than 25% of cleft surgeons report using the NAM appliance more than 50% of the time.14 Families often see the results of PSIO on social media and support-group websites, and may seek cleft teams that offer this treatment. Although it is not an ideal approach for all patients, NAM’s rising popularity is giving new prominence to the dentist’s role in the fabrication, adjustment and maintenance of these appliances.
DENTAL CARE BEYOND INFANCY
The NAM appliance or other PSIO modality is used continuously from the time of fabrication until the first surgical intervention to close the soft tissues of the lip, which usually takes place between 3 and 6 months of age. Following the initial surgery, PSIO appliances are no longer needed, and the role of the dental provider shifts to the more traditional tasks of providing anticipatory guidance and preventive care.
Children with cleft lip and/or palate often suffer from myriad dental anomalies in both primary and permanent dentitions.15 Supernumerary teeth and missing teeth are more likely in this population. Eruption of teeth, both primary and permanent, may be abnormal in and around the area of the hard tissue cleft. Teeth adjacent to the cleft have a higher incidence of malformation and malposition, and frequently require restoration due to caries or esthetic concerns (Figures 10A and 10B).

These malformations and defects tend to be more severe in the permanent dentition. Tooth problems, such as hypoplastic enamel, coupled with malposition and rotations, make teeth difficult to clean, predisposing children with clefts to caries. If the cleft is part of a larger syndrome, it is also possible there may be issues with dexterity and the ability to brush effectively.16,17 For these reasons, the role of the dental provider is vital for maintaining the function and integrity of the dentition as the child transitions from predentate to primary dentition — and eventually into young adulthood.
Beyond the scope of this review — but certainly a major concern for children with cleft lip and/or palate — is the need for orthodontic care. Due to malposed teeth, constricted arches and missing teeth, children with clefts will almost certainly require orthodontic appliances and, depending on severity, may require orthognathic surgery to maximize form and function of the dentition. A pediatric or general dentist may play a role in this orthodontic care.
CONCLUSION
Under a collaborative approach to treating cleft lip and/or palate, the role of the dental team has become more prominent with the rise of PSIO — but the importance of the dental provider remains integral over time. Monitoring teeth for proper eruption, making appropriate and timely referrals to orthodontic providers, and ensuring that families have established relationships with local cleft lip and palate teams are all vital functions. The American Academy of Pediatric Dentistry defines a dental home as “the ongoing relationship between the dentist and the patient, inclusive of all aspects of oral health care delivered in a comprehensive, continuously accessible, coordinated and family-centered way.” Nowhere is this definition more apt or important than when treating a child with cleft lip and/or palate.
REFERENCES
- World Health Organization. Global registry and database on craniofacial anomalies. Report of a WHO Registry Meeting on Crainofacial Anomalies. Available at: who.int/genomics/anomalies/en/CFA-RegistryMeeting-2001.pdf. Accessed October 17, 2017.
- Parker SE, Mai CT, Canfield MA, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004–2006. Birth Defects Res A Clin Mol Teratol. 2010;88:1008–1016.
- Wayne C, Cook K, Sairam S, Hollis B, Thilaganathan B. Sensitivity and accuracy of routine antenatal ultrasound screening for isolated facial clefts. Br J Radiol. 2002;75:584–589.
- James JN, Schlieder DW. Prenatal counseling, ultrasound diagnosis, and the role of maternal-fetal medicine of the cleft lip and palate patient. Oral Maxillofac Surg Clin North Am. 2016;28:145–151.
- Christ JE, Meininger MG. Ultrasound diagnosis of cleft lip and cleft palate before birth. Plast Reconstr Surg. 1981;68:854–859.
- McNeil C. Orthodontic procedures in the treatment of congenital cleft palate. Dent Rec (London). 1950;70:126–132.
- Latham RA, Kusy RP, Georgiade NG. An extraorally activated expansion appliance for cleft palate infants. Cleft Palate J. 1976;13:253–261.
- Pool R, Farnworth TK. Preoperative lip taping in the cleft lip. Ann Plast Surg. 1994;32:243–249.
- Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Clin Plastic Surg. 2004;31:149–158.
- Matsuo K, Hirose T, Tomono T, et al. Nonsurgical correction of congenital auricular deformities in the early neonate: a preliminary report. Plast Reconstr Surg. 1984;73:38–51.
- Kenny FM, Angsusingha Stinson D, Hotchkiss J. Unconjugated estrogens in the perinatal period. Pediatr Res. 1973;7:826–831.
- Garfinkle JS, King TW, Grayson BH, Brecht LE, Cutting CB. A 12-year anthropometric evaluation of the nose in bilateral cleft lip-cleft palate patients following nasoalveolar molding and cutting bilateral cleft lip and nose reconstruction. Plast Reconstr Surg. 2011;127:1659–1667.
- Sischo L, Clouston SA, Phillips C, Broder HL. Caregiver responses to early cleft palate care: a mixed method approach. Health Psychol. 2015; 35:474–482.
- Sitzman TJ, Girotto JA, Marcus JR. Current surgical practices in cleft care: unilateral cleft lip repair. Plast Reconstr Surg. 2008;121:261e–270e.
- Tannure NP, Oliveira CA, Maia LC, Vieira AR, Granjeiro JM, Costa Mde C. Prevalence of dental anomalies in non-syndromic individuals with cleft Lip and alate: a systematic review and meta-analysis. Cleft Palate Craniofac J. 2012;49:194–200.
- Ahluwalia M, Brasilsford SR, Tarelli E, et al. Dental caries, oral hygiene, and oral clearance in children with craniofacial disorders. J Dent Res. 2004;83:175–179.
- Lucas VS, Gupta R, Ololade O, Gelbier M, Roberts GJ. Dental health indices and caries associated microflora in children with unilateral cleft lip and palate. Cleft Palate Craniofacial J. 2000;37:447–452.
From Decisions in Dentistry. November 2017;3(11):35–38.