
Competence in Endodontic Treatment Planning And Prognosis
Following an accurate diagnosis, careful treatment planning will enhance the delivery of appropriate endodontic care and lead to optimal outcomes.
Second in a two-part series: The material in this multipart series was adapted from a white paper published in 2017 by the American Association of Endodontists. Appearing in the April 2018 issue, Part 1 outlined strategies for effective endodontic diagnosis, and is available at decisionsindentistry.com.
In parallel with the first installment of this two-part series, the American Association of Endodontists (AAE) offers this overview of endodontic treatment as a guideline for practitioners who undertake endodontic care. While the first part covered effective diagnosis, this article will examine endodontic treatment planning and prognoses. Before considering therapy, however, clinicians should understand that general dentists are bound to the same standard of care as endodontic specialists. Only if practitioners are confident they can meet this standard should treatment be rendered; otherwise, referral to an endodontist is recommended.
In the determination of whether to initiate treatment or refer:
- Clinicians should use the AAE Case Difficulty Assessment Form (CDAF) and guidelines (available at AAE.org) to establish a rationale for appropriate treatment and/or assess the need for referral due to anticipated case complexity. Practitioners should be able to apply the established criteria to each individual case and determine the degree of difficulty in providing nonsurgical or surgical root canal treatment.
- In the diagnosis and appropriate treatment of root resorption as a sequelae of trauma, clinicians should be capable of making a differential diagnosis of the types of root resorption, and be knowledgeable of the proper management for resorptive lesions, including referral to a dental specialist (as necessary) after appropriate imaging — including three-dimensional (3D) imaging technologies.
Guidelines utilized in endodontic treatment planning are designed to describe the clinical quality and professional performance of a procedure, without regard to the practitioner being a general dentist or specialist. Clinicians are encouraged to provide endodontic treatment consistent with their education, clinical experience and contemporary standards. The standard of practice and best practices for various services may change with time, and it is the provider’s responsibility to be aware of such changes.
The practitioner, when confronted with a case beyond his or her capabilities, has the following options and ethical responsibilities:
- Discuss all relevant benefits and risks of treatment options and limitations with the patient, ensuring that the information is understood before the patient is asked to provide informed consent.
- Refer the patient for consultation and/or treatment to an endodontist.
- Upgrade one’s skills to meet the standard of practice, as determined by the endodontic specialty.

and #31 in a patient referred for endodontic
treatment after the general dentist suspected
complex anatomy in both teeth. FIGURES 1 TO 4 COURTESY AHMED SALMAN, DDS
Endodontic procedures based on an established treatment plan should be of such quality that predictable and favorable results will routinely occur. Consideration must always be given to various treatment modalities that meet the standard of practice, but are favored by individual practitioners. Patients should be cognizant that any treatment modality, however acceptable, may not achieve an acceptable treatment outcome in every case. There are a number of factors — including biologic, intrinsic and psychological — that may preclude a successful result. These include the preexisting state of the patient’s medical and dental condition, patient compliance and follow-through, and complications and recognized risks of the procedures being performed.
In traumatic dental injuries, for instance, diagnosis and treatment are often complex, time consuming, expensive and may require a multidisciplinary approach. All dental professionals are expected to accurately diagnose, provide appropriate emergency care, and develop a treatment plan for traumatically injured teeth and their supporting structures. Providing urgent/emergent treatment that is inappropriate, for example, may compromise long-term outcomes.
All departures from expected outcomes should be noted in the patient’s record at the time of service, and the patient should be advised of compromised results as soon as the dentist is aware of the facts. In these circumstances, all information presented to the patient must be documented.
CASE ASSESSMENT
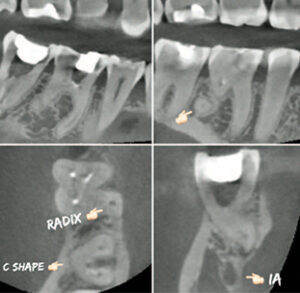
computed tomography identified tooth #30
as a radix entomolaris (disto-lingual root)
and #31 with C-shaped pulpal anatomy.
Many factors influence the degree of difficulty and risks of endodontic treatment. Recognition of these factors prior to the initiation of treatment helps patients and practitioners understand the complexities that may be involved in a given case. Endodontic treatment on a hopeless tooth is just as unethical as extracting a restorable tooth and replacing it with an implant.
The CDAF is a practical tool that makes case selection efficient, consistent and easy to document, providing a road map for when a generalist should treat or refer to an endodontist (Figure 1 through Figure 4). The CDAF specifically states that “technology, instruments and materials are not a replacement for clinical skill and experience, but, rather, adjuncts that a practitioner can employ to reach a desired goal.” The CDAF is intended to assist practitioners with endodontic treatment planning, but can also be used to help with referral decisions and record keeping. The assessment form identifies three categories that may affect treatment complexity: patient considerations, diagnostic and treatment considerations, and additional considerations. Within each category, levels of difficulty are assigned based on potential risk factors.
The levels of difficulty — ranging from minimal to moderate, as well as high difficulty — are sets of conditions that may not be controllable by the dentist. General practitioners who provide endodontic care should be competent to treat minimal-difficulty cases, and experienced general dentists may treat moderate-difficulty cases, but should always consider referral of these cases, as well as high-difficulty cases, to endodontic specialists. It is crucial that all dental providers recognize the limits of their skill and expertise in order to protect patients and provide quality care. Patient considerations that may complicate treatment include medical issues, difficulties with anesthesia, behavioral management issues, limited opening, and treatment complications. Additional considerations include previous endodontic treatment, a history of trauma, and periodontal/endodontic conditions.
Because endodontists set the standard of practice for conventional endodontics, if this standard cannot be met — such as the need for microscopy, performing regenerative procedures, treating complex traumatic injuries, 3D imaging for complex anatomy, or the need for apical surgery — the generalist should refer the patient to an endodontist. Planned endodontic treatment should not be doomed to failure due to a lack of understanding of what is required to provide quality care. For example, implants should never become an insurance policy for inadequate endodontic treatment.
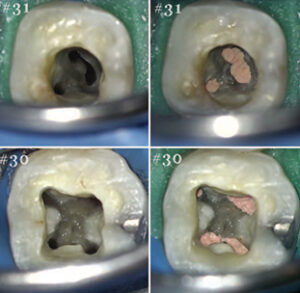
anatomy of teeth #30 and #31 seen in Figure 2.
ENDODONTIC TREATMENT PLAN
Once an endodontic problem has been confirmed, the practitioner must develop a course of action that will eliminate the cause, and have a favorable prognosis and long-term outcome. Treatment is based on a thorough understanding and interpretation of all diagnostic information, including patient history, clinical and radiographic data, and the strategic importance of the tooth/teeth being considered. Other factors include treatment complexities, anatomic complexities, periodontal status, and the structural integrity and restorability of the tooth. Clinicians must also take into account the prognosis and patient factors, such as age, attitude, motivation, anxiety, limited jaw opening, gag reflex, and the administration of antibiotics, analgesics and/or anti-inflammatory agents (when appropriate).
Though the final decision will rest with the patient, the treatment plan must include all options. It should be presented in language the patient understands, and provide valid reasons (based on the conditions) regarding which option is best, how the procedure will be done, how long it will take, what prognosis should be expected, and how much it will cost. The manner in which a case is presented should always be geared toward what is best for the patient. In many situations, the dentist should be in communication with the endodontist prior to even proposing treatment options to the patient.
RESTORABILITY
As part of the diagnosis and treatment planning process, careful consideration should be given to the final restoration. Studies suggest that the long-term prognosis for an endodontically treated tooth is equally dependent on the coronal restoration, as well as the quality of the endodontic treatment itself. Patients are not well served if the endodontic treatment is successful, but the tooth fails — and it has been demonstrated that loss of the coronal seal will result in a rapid recontamination of the root-canal-treated tooth.

of the dentition seen in Figure 1.
In recent years, there has been a major change in philosophy regarding the restoration of endodontically treated teeth. Researchers and clinicians have begun to realize the importance of respecting the preservation of tooth structure and the biological properties of the components of the tooth, namely, enamel, dentin and cementum. Minimal tooth structure should be removed while achieving all of the goals of debridement, disinfection and obturation.
Before commencing endodontic treatment, the clinician must consider a number of factors regarding restoration of the tooth; these include:
- The altered physical properties of tooth tissues following endodontic treatment
- Amount of dentin that will remain following caries and/or restoration removal and access cavity preparation
- Existence of a fracture/crack, and the extent of the fracture/crack
- Functional demands that will be placed on the restored tooth
- Clinical feasibility of ensuring that biologic width can be respected when the new restoration is placed with an adequate ferrule
- Likelihood of restoring or maintaining the ideal embrasure space and emergence profile
- The patient’s understanding that endodontic treatment is not complete until the permanent restoration is placed
Much has been written about the structural integrity and strength of the endodontically treated tooth. It is widely believed that endodontically treated teeth must be restored to improve the prognosis and are prone to fracture. Possible reasons for this include:
- Weakening of the tooth due to loss of tooth structure, especially loss of marginal ridges
- Alteration in the physical properties of the tooth due to the effects of chemical irrigants, such as hypochlorite and ethylenediaminetetraacetic acid
- Microbial factors, including the effects of bacteria/dentin interactions
- Restorative factors (for example, the effect of post-core restorations)
- Age factors, and the effect of age changes on dentin
TRAUMATIC DENTAL INJURIES
Managing dental trauma remains a significant clinical challenge that affects all dental professionals. Falls, accidents and sport-related injuries are the most frequent causes of dental trauma, with an estimated prevalence of 30%. Patients can present with a wide variety of injuries, ranging from crown or root fractures to trauma of the supporting periodontal structure, including luxations and avulsions. Treatment is often complex, time consuming, expensive, and will necessitate a multidisciplinary approach, such as endodontic and periodontal treatment, surgery, or orthodontic movements, as well as esthetic coronal restoration. Pulp necrosis, root resorption and ankylosis are the most common sequelae presenting major clinical challenges; this is due to the high risk of infraposition and underdevelopment of the alveolar bone. The general dentist should be knowledgeable about the prevention, diagnosis and treatment of traumatized teeth, including the need for advanced 3D technology for diagnosis and treatment planning. Outcome expectations of traumatized teeth are different than for nontraumatized teeth.
INFORMED CONSENT
After an endodontic diagnosis is made, the benefits, risks, treatment plan, and alternatives to endodontic treatment — including any patient refusal of recommended treatment and the consequences of refused treatment — should be presented to the patient or the patient’s guardian. Clinicians should document acceptance or informed refusal of treatment recommendations. The patient or guardian, along with a witness (who can be a staff member), should sign and date the consent form. Upon informing the patient of the diagnosis, recommended treatment plan, prognosis and risks, the provider’s responsibility is satisfied. A practitioner cannot be forced to perform dental services that he or she deems contrary to the patient’s overall health. In short, the right of the patient to accept treatment is balanced by the right of the dentist to refuse treatment when both parties understand the rational consequences of their actions.
PROGNOSTIC COMPETENCE
In determining prognosis for endodontic treatment, the dentist should be able to forecast the outcome of initial nonsurgical root canal treatment, based on the pulp and periapical diagnosis, tooth anatomy and morphology, remaining tooth structure, and periodontal support. In addition, the clinician should be able to assess treatment outcomes through clinical and radiographic measures, and identify healing versus nonhealing of nonsurgical root canal treatment. When nonhealing occurs, the dentist should be capable of identifying the etiology and recommend corrective treatment strategies or refer to an appropriate dental specialist.
Stedman’s Medical Dictionary defines prognosis as “a forecast of the probable course and/or outcome of a disease.” Establishing a prognosis is not an exact science; even cases that appear favorable — and in which treatment meets the accepted standard of practice — can have unfavorable outcomes. It is unrealistic to expect that all endodontic treatment will be successful. This process requires the clinician to have (1) a broad understanding of evidence-based dentistry, (2) the ability to collect all relevant clinical information, (3) an understanding of all treatment options, and (4) the capability to effectively communicate with the patient and appropriate specialists. In addition, providers of endodontic therapy must act in a professional and ethical manner that promotes the patient’s best interest.
Establishing a prognosis is essential prior to treatment, during treatment, following treatment, and upon recall examination. The prognosis is unique to the patient and clinician providing care. Subsequent to obtaining a diagnostic database, the general dentist must conduct a case difficulty assessment, evaluate the knowledge and clinical skill required to perform the procedure, and, in difficult cases, consider specialty care to enhance the prognosis.
Interdisciplinary care can improve patient outcomes, and the use of enhanced technologies, such as microscopy, 3D imaging, ultrasonics, regenerative procedures and osteo-inductive materials, can further enhance the prognosis of endodontic cases.
PRETREATMENT PROGNOSIS
To establish a pretreatment diagnosis, treatment plan and prognosis, clinicians must have an understanding of clinical and radiographic criteria for determining pulpal and periradicular pathoses, and be able to differentiate these from nonendodontic pathoses. Endodontic providers must also demonstrate detailed knowledge of potential lesions that can mimic endodontic pathoses, and be capable of establishing an etiology for pulpal pathoses to include caries, trauma, developmental defects, coronal cracks/fractures, resorptive lesions, periodontal pathosis, and restorative procedures. In addition, practitioners must be proficient in identifying the clinical signs and symptoms of pulpal and periapical pathoses from nonendodontic pathoses, and interpreting normal/abnormal test results and clinical findings. A detailed knowledge of pulp and periradicular anatomy and morphology and variations by tooth group is required, as is understanding the case difficulty assessment criteria and knowing when to refer a case to a specialist.
POSTTREATMENT PROGNOSIS
Following nonsurgical treatment, the clinician must have an understanding of the criteria for successful therapy; this includes clinical monitoring of the patient’s signs and symptoms, identifying iatrogenic incidents during treatment (such as missed canals, loss of length, ledges, apical transportation, apical, lateral and furcal perforations, or fractured instruments), and evaluating the quality of obturation, including adequate length, density, taper and coronal seal.
OUTCOME ASSESSMENT (ONE YEAR AND BEYOND)
Additionally, the clinician must have an understanding of clinical and radiographic criteria for determining success or nonhealing following endodontic treatment. This includes the ability to recognize clinical signs and symptoms of pulpal and periapical pathoses, and normal/abnormal test results and clinical findings. It also requires competence in evaluating radiographic evidence of pathoses and/or osseous regeneration, as well as radiographic evidence of procedural errors in endodontic and restorative treatment (including coronal leakage).
The treatment options for cases in which nonhealing has been established should include nonsurgical retreatment, root-end surgery, perforation repair, guided tissue regeneration, hemi-section and root amputation, intentional replantation, extraction and no treatment.
MEASURING COMPETENCE
Competence in endodontic prognosis and outcome assessment is demonstrated by the following knowledge, skills and behaviors. Providers should be able to:
- Describe prognosis and outcome assessment, based on the best-available current evidence
- Recognize restorability of a tooth and possible need for crown lengthening
- Evaluate the patient’s periodontal status
- Assess the quality of previous endodontic treatment
- Identify past traumatic dentoalveolar injuries
- Recognize the presence of incomplete crown/root fractures
- Assess the presence of internal or external root resorption
- Explain the benefits, risks, alternatives and prognosis of treatment options in terms that are appropriate to patient’s background and knowledge of dentistry
- Compare prognoses and the cost effectiveness of initial root canal treatment, retreatment, surgical treatment and tooth replacement options
- Explain the difference between success and survival as outcome measures
- Determine patient preference regarding treatment options
- Evaluate immediate posttreatment outcomes, and explain the influence of procedural errors, missed canals, quality of obturation, and significance of coronal restoration to long-term outcomes
- Assess posttreatment healing and recognize situations in which referral for possible treatment revision and/or surgery is indicated
- Describe potential causes of persistent pain following root canal treatment, and explain diagnostic tests and methods to distinguish between pain of odontogenic and nonodontogenic origin
CONCLUSION
These guidelines are intended to help dental professionals understand the knowledge and skills required of all practitioners — general dentists and endodontists alike — who provide endodontic treatment. Such therapy should only be rendered by those who are able to meet today’s standard of care, as established by the AAE. An accurate diagnosis provides the foundation for effective endodontic treatment planning and therapy — and demonstrating competence in all three areas is key to ensuring optimal outcomes.
KEY TAKEAWAYS
- Before considering endodontic treatment, clinicians should understand that general dentists are bound to the same standard of care as endodontic specialists.
- Practitioners are encouraged to provide endodontic treatment consistent with their education, experience and contemporary standards, and be ready to refer cases that are beyond their skill level.
- Dentists should use the American Association of Endodontists Case Difficulty Assessment Form and guidelines (available at AAE.org) to establish a rationale
for treatment or assess the need for referral. - Demonstrating competence in endodontic diagnosis, case planning, treatment and prognosis is key to providing safe and effective care.
SUGGESTED BIBLIOGRAPHY
Treatment Planning, Retreatment, Microsurgery, Decision-Making
- Venskutonis T, Plotino G, Juodzbalys G, Mickeviciene L. The importance of cone beam computed tomography in the management of endodontic problems: a review of the literature. J Endod. 2014;40:1895–1901.
- Ee J, Fayad MI, Johnson BR. Comparison of endodontic diagnosis and treatment planning decisions using cone-beam volumetric tomography versus periapical radiography. J Endod. 2014;40:910–916.
- Andersson L, Andreasen JO, Day P, Heithersay G, Trope M, Diangelis AJ, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent Traumatol. 2012;28:88–96.
- Diangelis AJ, Andreasen JO, Ebeleseder KA, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28:2–12.
- Malmgren B, Andreasen JO, Flores MT, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 3. Injuries in the primary dentition. Dent Traumatol. 2012;28:174–182.
- American Association of Endodontists. The recommended guidelines of the American Association of Endodontists for the treatment of traumatic dental injuries. Chicago, IL: 2013;1–16.
- Cohenca N, Simon JH, Roges R, Morag Y, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 1: traumatic injuries. Dent Traumatol. 2007;23:95–104.
- Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K. Outcome of primary root canal treatment: systematic review of the literature — Part 1. Effects of study characteristics on probability of success. Int Endod J. 2007;40:921–939.
- Lazarski MP, Walker WA 3rd, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of nonsurgical root canal treatment in a large cohort of insured dental patients. J Endod. 2001;27:791–796.
- Salehrabi R, Rotstein I. Endodontic treatment outcomes in a large patient population in the USA: an epidemiological study. J Endod. 2004;30:846–850.
- Gilbert GH, et al. Outcomes of root canal treatment in Dental PBRN practices. Gen Dent. 2010;58:28–36.
- Del Fabbro M, Taschieri S, Testori T, Francetti L, Weinstein RL. Surgical versus non-surgical endodontic re-treatment for periradicular lesions. Cochrane Database of Systematic Reviews. 2007;Issue 3:Art. No. CD005511.
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009;35:930–937.
- Ng YL, Mann V, Gulabivala K. Outcome of secondary root canal treatment: a systematic review of the literature. Int Endod J. 2008;41:1026–1046.
- Salehrabi R, Rotstein I. Epidemiological evaluation of the outcomes of orthograde endodontic retreatment. J Endod. 2010;35:790–2.
- Panitvisai P, Parunnit P, Sathorn C, Messer HH. Impact of a retained instrument on treatment outcome: a systematic review and meta-analysis. J Endod. 2010;36:775–780.
- Setzer F, Shah S, Kohli M, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature — Part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010;36:1757–1763.
- Setzer F, Kohli M, Shah S, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature — Part 2: Comparison of endodontic microsurgical techniques with and without use of higher magnification. J Endod. 2012;38:1–10.
- Tsesis I, Rosen E, Tamse A, Taschieri S, Del Fabbro M. Effect of guided tissue regeneration on the outcome of surgical endodontic treatment: a systematic review and meta-analysis. J Endod. 2011;37:1039–1045.
- Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M. Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod. 2013;39:332–339.
- Kang M, In Jung H, Song M, Kim SY, Kim HC, Kim E. Outcome of nonsurgical retreatment and endodontic microsurgery: a meta-analysis. Clin Oral Invest. 2015;19:569–582.
- Zitzmann NU, Krasti G, Hecker H, Walter C, Waltimo T, Weiger R. Strategic considerations in treatment planning: deciding when to treat, extract, or replace a questionable tooth. J Prosthet Dent. 2010;104:80–91.
Outcomes, Risk Factors, Prognosis, Implants
- Burry JC, Stover S, Eichmiller F, Bhagavatula P. Outcomes of primary endodontic therapy provided by endodontic specialists compared with other providers. J Endod. 2016;42:702–705.
- Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 2006;13:57–83.
- Vaz de Souza D, Schirru E, Mannocci F, Foschi F, Patel S. External cervical resorption: a comparison of the diagnostic efficacy using 2 different cone-beam computed tomographic units and periapical radiographs. J Endod. 2017;43:121–125.
- Cohenca N, Simon JH, Mathur A, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma. Part 2: root resorption. Dent Traumatol. 2007;23:105–113.
- De Paula-Silva FW, Wu MK, Leonardo MR, Bezerra da Silva LA, Wesselink, PR. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod. 2009;35:1009–1012.
- Peters CI, Peters OA. Cone beam computed tomography and other imaging techniques in the determination of periapical healing. Endod Topics. 2013;29:57–75.
- Giannobile WV, Lang NP. Are dental implants a panacea of should we better strive to save teeth? J Dent Res. 2016;95:5–6.
- Torabinejad M, Anderson P, Bader J, et al. Outcomes of root canal treatment and restoration, implant supported single crowns, fixed partial dentures, and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98:285–311.
- Torabinejad M, Landaez M, Milan M, et al. Tooth retention through endodontic microsurgery or tooth replacement using single implants: a systematic review of treatment outcomes. J Endod. 2015;41:1–10.
- Doyle SL, Hodges JS, Pesun IJ, Law AS, Bowles WR. Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod. 2006;32:822–827.
- Doyle SL, Hodges JS, Pesun I, Baisden MK, Bowles WR. Factors affecting outcomes for single-tooth implants and endodontic restorations. J Endod. 2007;33:399–402.
- Iqbal MK, Kim S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod. 2008;34:519–529.
- Morris MF, Kirkpatrick TC, Rutledge RE, Schindler WG. Comparison of nonsurgical root canal treatment and single-tooth implants. J Endod. 2009;35:1325–1330.
- Zitzmann NU, Krasti G, Hecker H, Walter C, Weiger R. Endodontics or implants? A review of decisive criteria and guidelines for single tooth restorations and full arch reconstructions. Int Endod J. 2009;42:757–774.
- Pennington MW, Vernazza CR, Shackley P, Armstrong NT, Whitworth JM, Steele JG. Evaluation of the cost-effectiveness of root canal treatment using conventional approaches versus replacement with an implant. Int Endod J. 2009;42:874–883.
- Kim SG, Solomon C. Cost-effectiveness of endodontic molar retreatment compared with fixed partial dentures and single-tooth implant alternatives. J Endod. 2011;37:321–325.
Featured image by YELO34/ISTOCK/GETTY IMAHES PLUS
From Decisions in Dentistry. June 2018;4(6):8–12.


