
Clinical Considerations For Cone Beam Computed Tomography
While three-dimensional imaging is a helpful diagnostic aid, like any form of radiography, it must be used judiciously.
In recent years, three-dimensional (3D) radiographic imaging has joined conventional two-dimensional (2D) imaging as viable radiographic modalities. Technically known as cone beam computed tomography (CBCT), 3D radiography was first introduced in Europe in 1998 and arrived in the United States in 2001.1 It now serves as an influential clinical tool in the diagnosis of various oral health conditions. As the technology has improved, CBCT has become an effective imaging modality that produces 3D views in any plane where visualization of the oral and maxillofacial structures is necessary. As the use of this technique continues to grow in private practice, dentists should be knowledgeable about its applications, and how these images can be incorporated into treatment planning.
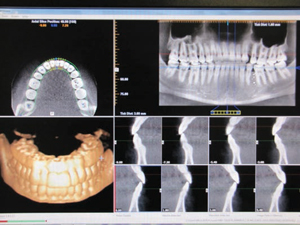
A cone beam scanner uses a cone shaped X-ray beam and a reciprocating, flat-panel detector that rotates around the patient 360 degrees and acquires between 150 and 1599 projected images.2 Scanning time ranges from five to 40 seconds, depending on the specific unit and settings.1 After the scan is complete, these incomplete images are processed by reconstruction to produce digital images in the form of units called voxels. The smallest subunits of digital images, voxels have equal parameters in all three dimensions and are stacked in rows and columns.1 The information is interpreted by software and organized to produce a 3D image from different perspectives (Figure 1 and Figure 2). With these data, dental professionals can visualize the information as reconstructed images. All other parameters of digital imaging, such as brightness, contrast and hue, can be adjusted for an optimal view of the processed image.3

A key advantage of CBCT scanning is that it takes less time than a routine computed tomography (CT) scan. The CBCT data only require a single rotation of the X-ray source, during which all of the needed images are procured. The time needed to acquire an image is less than a minute, but the reconstruction of the image can take considerably longer.4 And because CBCT scans take less time to capture than CT scans, radiation dose is also decreased. A full field view CBCT image requires a radiation dose of 29 µSv to 477 µSv.4 Compared to a conventional CT scan, CBCT imaging reduces radiation emission from 1.3% to 22.7%.4
Another advantage of CBCT imaging is that its voxel resolution is able to produce accuracy in all dimensions of the image. In addition, the collimation used in this technology enables the X-ray beam to be focused only on areas of interest — thus, clinicians can select the optimal level of radiation frequency, depending on what needs to be imaged.4 This modality also produces images in all three planes of space, which is not possible in intraoral or panoramic radiographs or cephalograms. Measurement algorithms, such as scaling and zooming, allow the clinician to highlight anatomic areas required for diagnosis.4
RESPECT THE LIMITATIONS
For all its benefits, there are limitations to using CBCT, including a lack of clarity with some images. Also, many pathologies can still be detected through the use of conventional radiographs, thus reducing the need for 3D imaging. Although radiation exposure is less than a CT scan, CBCT imaging still exposes the patient to more radiation than a traditional full mouth series of radiographs. The clarity of CBCT images is affected by artifacts, which are radiographic factors from the CBCT unit that contribute to loss of detail and lead to a grainy appearance of the image, or noise, and poor soft tissue contrast.5
Artifacts are the distortions of images that are not present and are not related to the subject. They are categorized into patient-related artifacts, scanner-related artifacts, and cone beam-related artifacts. They can be reduced by collimation, modified patient positioning, separation of dental objects, and introducing certain algorithms.5 Patient movement during scanning can degrade image sharpness and increase distortion. These errors can be reduced by implementing a shorter scanning time and by using a head restraint. In addition, metallic objects or dental restorations in the patient can cause streak artifacts on the image. Poor calibration and scanner detection imperfections can lead to a circular or ring-shaped artifact being imposed on the image. Improper image processing and image reconstruction errors can also produce streaking artifacts, image distortion and noise.5,6
key takeaways
- Cone beam computed tomography (CBCT) has become an effective imaging modality that produces threedimensional views in any plane where visualization of the oral and maxillofacial structures is necessary.
- Beside surgery, CBCT has applications in orthodontics, endodontics, implantology, periodontics and other therapies.
- When compared to conventional two-dimensional imaging, such as panoramic radiographs and full mouth series, CBCT produces greater radiation exposure, so its use must be justified.2
- The collimation used in this technology enables the X-ray beam to be focused only on areas of interest — thus, clinicians can select the optimal level of radiation frequency, depending on what needs to be imaged.4
- While CBCT has many uses in dentistry, it is not always the primary imaging choice. This is not a replacement for conventional radiographs, and should only be utilized when traditional radiographs cannot help provide an accurate diagnosis.
APPLICATIONS IN CLINICAL PRACTICE
Initially, the use of CBCT was confined to surgical assessment of oral and maxillofacial pathologies and reconstruction. Later uses of CBCT expanded to orthodontics, endodontics, caries detection, implant diagnosis, temporomandibular joint (TMJ) assessment, preoperative and postoperative assessment of craniofacial fractures, salivary gland imaging and periodontics. While CBCT can be used in these instances, it is not always the primary choice. This is not a replacement for routine 2D radiographs, and should only be utilized when conventional radiographs cannot help provide an accurate diagnosis.
In orthodontic applications, CBCT can enhance volumetric analysis by providing a clear distinction between soft tissue of the pharynx and the airway space. Analyzing airway space and craniofacial growth patterns are important considerations when providing orthodontic treatment. Other uses of CBCT in orthodontics can include locating impacted teeth, determining cortical plate location with regards to root position and torque, and locating a temporary anchorage device after it’s been placed. This imaging modality can be used with computer software for enhanced analysis of therapeutic results, possibly contributing to shorter treatment times. An orthodontist can also relate the occlusal plane of view to the condyles with the TMJ fossa, and can compare the dental arches with the other hard and soft tissues surrounding it.7
Along the same lines, CBCT has proved to be a helpful diagnostic tool in endodontic practice because of the 3D information it provides. According to a study by Cheng et al, the evaluation of root canal obturation length by CBCT in comparison with periapical radiography showed that CBCT is the best method for the initial identification of maxillary first molar internal morphology.8 It can be used to observe the sagittal, coronal and axial planes to determine if root canal obturation is overextended or underextended. It can be used to locate the apical foramen and therefore diagnose obturation lengths. This is a major advantage when compared to periapical radiography.8
This sophisticated imaging technology is likewise helpful for surgical assessment of pathologies. The assessment of complicated third molar impactions necessitates a 3D view in order to interpret the adjoining structures involved. Sumomalainen et al found that CBCT is more effective than 2D radiography in assessing the complicated root morphology, root structure variations, and their corresponding structures before surgical extraction of impacted teeth.9,10 It also provides superior sensitivity values, specificity values and prediction values. The 3D reconstruction of the bony structures illustrates tumor invasion into the surrounding structures and helps to localize the tumors with exact boundaries, assisting in surgical assessment.11
The use of 3D imaging techniques has improved the accuracy of diagnosis and treatment planning for dental implant placement. The CBCT scan improves visualization of the anatomy, and the relationships of implants with adjacent structures. These images also provide a detailed view of implant sites, allowing the practitioner to consider all relative parameters, including facio-lingual/mesio-distal widths, grafted bone, density of bone, and concavity of bone.12
The use of 3D imaging techniques has improved the accuracy of diagnosis and treatment planning
When it comes to caries diagnosis, CBCT is best used to determine the depth of interproximal and occlusal lesions. There is a chance for false positives due to an increase in sensitivity and decrease in specificity with the CBCT unit. This modality cannot be used on restored teeth that contain metal or radiopaque material, however, due to concerns they may cause streak artifacts in the images. When using CBCT for caries diagnosis, a bitewing radiograph is also needed for precise diagnosis.13 Although caries can sometimes be interpreted using a CBCT image, intraoral radiographs are still the best choice for caries diagnosis.
Although many of the same items can be interpreted on conventional 2D radiographs and CBCT images, 3D imaging provides increased detail in periodontic applications, including details of buccal and lingual defect measurements.14 In addition, CBCT offers a better visual appearance of intrabony defects, as well as dehiscence and fenestration defects, periodontal cysts and furcation-involved molars.15
CONCLUSION
Due to its enhanced diagnostic capabilities and the decreasing cost of CBCT units, the use of this technology is increasing in both private practice and dental schools. Yet when compared to conventional imaging, such as panoramic radiographs and full mouth series, CBCT produces greater radiation exposure, so its use must be justified.2 As with all dental radiographs, CBCT images should only be taken when needed and not overprescribed. Adequate training of dental personnel is also key.16 A patient’s dental and health history should be thoroughly evaluated in conjunction with a clinical exam. Once this evaluation has been completed, conventional radiographs and/or CBCT imaging can be prescribed, based on patient need.
This imaging modality should only be used for specific cases in which 3D views are superior to conventional radiography — such as demonstrating the location and extent of pathology, the quantity and quality of bone, and the spatial relationship of an object relative to the adjacent critical anatomical structures.2 Clinicians should review the American Dental Association’s parameters for incorporating CBCT into daily practice.17
Although CBCT imaging provides a unique perspective of the oral cavity, it is not needed for all patients. As with any radiographic exposure, clinicians should be guided by the “as low as reasonably achievable” (ALARA) principle when prescribing 3D images. The decision to utilize this technology should be based on a review of the patient’s medical and dental history, in conjunction with a thorough clinical exam. After routine radiographs are taken, if a different vantage point is needed for diagnosis or treatment, a CBCT image can provide enhanced viewing capabilities under certain parameters. But because 3D radiography emits higher doses of radiation than conventional imaging, its use should be limited. All dental personnel using CBCT should receive proper training to ensure the safety of both patients and clinicians.
References
- Hatcher, DC. Operational principles for conebeam computed tomography. J Am Dent Assoc. 2010;141:3S–6S.
- Adibi S, Zhang W, Servos T, O’Neill PN. Cone beam co mputed tomography in dentistry: what dental educators and learners should know. J Dent Educ. 2012;76:1437–1441.
- Sukovic, P. Cone Beam Computed Tomography in Dentomaxillofacial Imaging. Available at: http://web.archive.org/web/20041122021652/http://www.aadmrt.org/currents/sukovic_winter_04_print.htm. Accessed November 13, 2015.
- Scarfe WC, Farman AG. Cone beam computed tomography: a paradigm shift for clinical dentistry. Australasian Dental Practice. 2007:102–110.
- Scarfe WC, Farman AG. What is cone beam CT and how does it work? Dent Clin North Am. 2008;52:707–730.
- Katsumata A, Hirukawa A, Noujeim M, et al. Image artifact in dental cone beam CT. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:652–657.
- Mah JK, Huang JC, Choo H. Practical applications of cone beam computed tomography in orthodontics. J Am Dent Assoc. 2010;141:7S–13S.
- Cheng L, Zhang R, Yu X, et al. A comparative analysis of periapical radiography and conebeam computerized tomography for the evaluation of endodontic obturation length. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:383–389.
- Suomalainen A, Ventä I, Mattila M, Turtola L, Vehmas T, Peltola JS. Reliability of CBCT and other radiographic methods in preoperative evaluation of lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:276–284.
- Pohlenz P, Blessmann M, Blake F, Heinrich S, Schmelzle R, Heiland M. Clinical indications and perspectives for intraoperative cone beam computed tomography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:412–417.
- Dreiseidler T, Alarabi N, Ritter L, et al. A comparison of multislice computerized tomography, cone beam computerized tomography, and single photon emission computerized tomography for the assessment of bone invasion by oral malignancies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:367–374.
- Worthington P, Rubenstein J, Hatcher DC. The role of cone beam computed tomography in the planning and placement of implants. J Am Dent Assoc. 2010;141:19S–24S.
- Tyndall DA, Rathore S. Cone beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am. 2008;52:825–841.
- Mol A. Imaging methods in periodontology. Periodontol 2000. 2004;34:34–48.
- Kasaj A, Willershausen B. Digital volume tomography for diagnostics in periodontology. Int J Comput Dent. 2007;10:155–168.
- Scarfe WC, Levin MD, Gane D, Farman AG. Use of cone beam computed tomography in endodontics. Int J Dent. 2009;2009:634567.
- The American Dental Association Council on Scientific Affairs. The use of cone beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143:899–902.


