
CE Sponsored by ZEISS in Partnership With the American Association of Endodontists — Benefits of Nonsurgical Endodontic Retreatment
Aided by advanced technology, nonsurgical revision increases tooth survival rates and improves patients’ quality of life.
PURCHASE COURSE
This course was published in the April 2017 issue and expires April 2020. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Describe the basis for nonhealing after initial root canal therapy.
- Explain the techniques and materials used in endodontic retreatment, as well as potential complications and risks.
- Identify the armamentarium needed for successful nonsurgical retreatment.
ZEISS is offering this CE course free to the first 300 online test-takers; enter code ZEISS417 at checkout.
Introduction
ZEISS enables health care professionals worldwide to improve the lives of their patients in ophthalmology, microsurgery, and other medical and dental growth sectors. We advance the standard of care with our proven medical technology and application competence.
We are inspired by a clear vision: ZEISS wants to be the partner of choice for general dentists and specialists. Being a partner means understanding all aspects of dental providers’ requirements and the challenges they face to help them succeed. Success means optimal treatment for patients. Success also means being cost-efficient, achieving predictable outcomes, or offering what other oral health professionals cannot.
Our surgical microscopes for dentistry help clinicians visualize details and fine structures that are otherwise difficult to see, therefore enhancing the quality of treatment across all disciplines. With the goal of improving outcomes in root canal therapy and endodontic restoration, ZEISS is delighted to support the development of this article with an unrestricted educational grant. We hope it encourages a multidisciplinary approach to treatment and helps raise clinicians’ level of care.
The American Association of Endodontists (AAE) is a global resource for knowledge, research and education for the oral health care profession, members and public. Our members rely on our innovative education, professional development opportunities and advocacy efforts to help them achieve clinical excellence and provide the highest levels of care.
The AAE is pleased to partner with Decisions in Dentistry to provide high-quality, clinical endodontic content — written by endodontists — to the broader dental profession. Nonsurgical endodontic retreatment is an important topic for today’s clinicians. Our members report increases in retreatment cases, which is telling because it means dentists see retreatment as a viable option to save the natural dentition; but this also accounts for unsuccessful initial root canal therapy. By partnering with an endodontist for treatment planning, general dentists and their patients will realize the best outcomes possible through initial treatment or retreatment, if necessary.
Teeth receiving contemporary endodontic therapy using accepted protocols, instruments and materials have an excellent survival rate. While this approach maintains tooth function and retention,1–3 initial root canal treatment may not always result in absolute healing or elimination of symptoms. Outcomes are influenced by a variety of clinical factors.
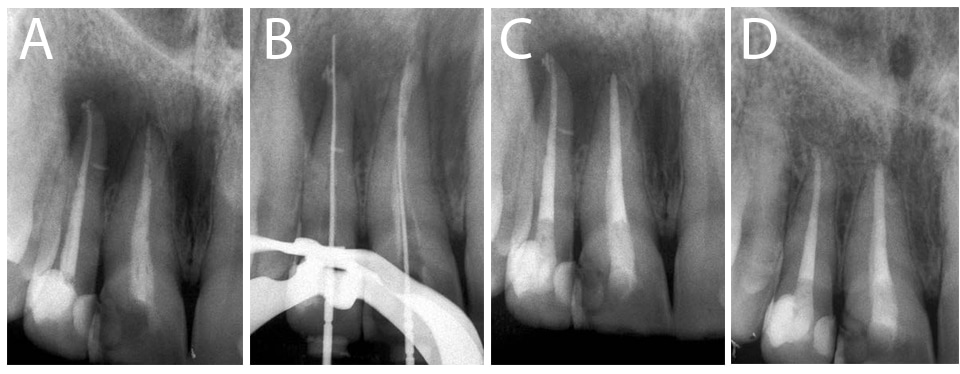
Initial therapy may fail due to an inability to completely remove microorganisms present at the time of treatment, or their reintroduction after completion of primary treatment.4–6 Pathogenic microbes can survive after initial treatment due to untreated or undetected canals, complex anatomical features or incomplete execution while cleaning and shaping.7–10 The reestablishment of microorganisms after the completion of initial treatment is essentially caused by recurrent caries and coronal microleakage (Figures 1A through 1C).11 Other factors that may contribute to nonhealing after initial nonsurgical root canal therapy include procedural errors, inadequate decay removal, anatomical anomalies, or intracanal and extraradicular biofilms.12 Procedural errors can result in perforations, canal transportation, instrument breakage or ledges.7,10,13 Moreover, primary orthograde treatment can be compromised by long-term use of temporary materials when definitive restorations are not provided within an acceptable time period.14–15

In the case of nonhealing, a combination of subjective clinical symptoms, radiographs and clinical findings can all contribute to a diagnosis that supports endodontic retreatment. Symptoms can include persistent discomfort from the previous treatment, biting pain, a history of swelling, sinus tract formation, or discomfort when palpating the vestibule. Imaging may reveal an increase in the size of a preexisting radiolucency or an emerging periapical lesion not evident during initial treatment. Typically, objective findings may include recurrent caries, defective or missing permanent or provisional restorations, and palpation and percussion sensitivity. Conventional radiographs or cone beam computed tomography (CBCT) may reveal poor root canal fillings with voids, short obturations, untreated canals, separated instruments, recurrent caries or defective restorations with open margins.16,17
Nonsurgical retreatment should be the principal option if the tooth is periodontally stable (without detectable root fractures) and exhibits adequate structure to provide access. After disassembly and caries removal, tooth assessment should entail periodontal probing, mobility and crown-to-root ratio determination, crown lengthening requirements, and the importance of the tooth in the overall treatment plan.9,10,18 If initial root canal treatment fails to promote healing, viable strategies include nonsurgical retreatment, periradicular surgery, intentional replantation or extraction. In cases in which the tooth is still restorable, nonsurgical retreatment or revision is the primary option for patients motivated to maintain their natural dentition. Surgical treatment should only be considered in the presence of canal obstructions, extensive fixed prosthetic appliances, or difficult-to-remove post and cores that make nonsurgical retreatment unfeasible. Nonsurgical retreatment is a strategy that increases success rates in nonhealing cases.19 Tooth extraction should be considered only if other therapies cannot be completed or the patient is unmotivated to preserve his or her natural dentition.7–9
A large percentage of retreatment cases are complex and require advanced instrumentation and training, partnered with use of the dental operating microscope (DOM).9,10,20 These challenging cases are routinely referred and performed by endodontists. Many nonsurgical revision cases, however, can be completed by general dentists with advanced education, experience and equipment. Case assessment is critical in determining which treatment option will most likely result in tooth retention.
Clinicians should inform patients the procedure is more complex than initial treatment, and may require multiple appointments. It is also essential that the operatory is equipped with a DOM, ultrasonic units with functional tips, conventional and retreatment files, rotary handpieces, solvents, dental dams, irrigation systems, and post-extraction and file-removal kits. Referral to an endodontist is recommended if the case is not within the clinician’s scope and training. The restorability of the tooth after disassembly is an additional consideration in nonsurgical endodontic revision. Nonsurgical retreatment is contraindicated when restorative materials, caries, and post and core removal compromise the remaining tooth structure and restorability is not attainable. Other considerations include teeth with poor crown-to-root ratios, advanced periodontal disease, root fractures, or patients with financial limitations or poor oral hygiene who are unmotivated to preserve natural dentition.9,10
SURGICAL INDICATIONS
Unremovable preformed cast posts and cores, anatomical obstructions, root canal calcifications or anatomical obstructions can be managed by initiating periradicular surgery.7,10 Additional indications for surgery in nonhealing cases include unremovable filling materials, root resorption, separated instruments that cannot be retrieved or bypassed, or some cases displaying periapical lesions larger than 5 mm.21,22 Furthermore, teeth exhibiting iatrogenic preparation errors — including ledging, perforations, transportation, or physiological external inflammatory root resorption that cannot be resolved with an internal approach — will require a surgical strategy.7,10 Advances in bioceramic materials can address some of these challenges by resolving pathosis with an orthograde approach that uses mineral trioxide aggregate (MTA) obturation, rather than conventional gutta-percha and sealer (Figures 2A through 2D).23
In accordance with informed consent and the standard of care, all treatment options must be offered to patients, who should be informed of the potential risks of nonsurgical retreatment. These include potential fracture of porcelain crowns or dislodgement, perforation or root fracture during post and core removal, or iatrogenic perforations generated during disassembly.9,10,24 In addition, treatment revision may further weaken the tooth and create ledges, canal transportation or instrument breakage. The major advantages of retreatment include retention (with continued function of the natural tooth), and avoiding more aggressive treatment — such as bridge or implant placement.
RETREATMENT PROCEDURES
Restoration Removal and Retention Criteria — The removal of the coronal restoration expedites and simplifies nonsurgical retreatment by allowing visualization (with the aid of the DOM) and access during disassembly.9,18,20 After complete removal of the coronal restoration, microleakage can be assessed subsequent to caries removal while inspecting the pulpal floor for fractures. If recurrent caries are evident when full-coverage restorations are present, complete crown removal and replacement are indicated. Anterior esthetic crowns that show acceptable marginal integrity (without recurrent caries) can be treated through a conservative lingual access opening.9,10,18 Large posts, however, will require crown removal and provisionalization to complete treatment. If retreatment can be completed without compromising the full-coverage restoration, the access cavity must be sealed with a bonded permanent restoration.
Canal Obstructions — In the presence of canal obstructions, unsuccessful negotiation of the canal system during retreatment can contribute to nonhealing. If tooth retention is the goal, a surgical approach is the primary option when obstructions are not removable and periapical pathosis is present. Canal obstructions include post and core restorations, calcifications, iatrogenic ledges, and separated instruments, silver points, metallic debris or carriers.7,9,10 Challenging cases may require referral to a specialist.25
Post and Core Removal — Nonsurgical retreatment often requires the disassembly of post and core restorations. The outcome depends on the expertise of the operator using the DOM and various ultrasonic systems (teamed with specifically designed tools).26 Factors that influence the outcome include the type of buildup material (cast versus preformed); diameter, length and location of the dowel; post composition (metallic or nonmetallic); and the bonding system or cement used. Some long and well-fitting metal, zirconium or fiber posts cemented with resin materials may be difficult, if not impossible, to remove.10,18,24 Their removal is contraindicated if the root structure is thin and likely to perforate or fracture.18,24 Incremental core removal requires the use of carbide, diamond or transmetal burs and specifically designed ultrasonic tips — visualized with the DOM — in order to conserve tooth structure while preserving the extruding coronal post segment. Following core removal, visible cement or composite surrounding the post can be circumferentially troughed and removed using fine ultrasonic tips.10,27
Using high energy settings, ultrasonic tips are used to loosen the post after the cement has been cleared. Since the procedure generates high temperatures, water coolants are recommended with ultrasonic energy directed in different locations at 15- to 20-second intervals around the exposed post.27–29 Without water coolants, root temperatures can increase 10°C and may induce supporting bone necrosis, with possible loss of the tooth.29 Post-removal time varies, depending on factors such as the length, width and type of post, plus the luting agent used.10,28,29 Loosened posts can be removed with small-tipped forceps, hemostats, pliers, or specially designed tapping devices (e.g., Ruddle Post Removal System).10,24,30,31 Once the post has been removed, excess cement or composite can be removed using solvents, hand or rotary instruments, and specific ultrasonic tips. In addition, post-removal kits are available featuring trefan burs with matched tapping extractors that allow safe removal while the remaining tooth structure is cushioned with rubber washers.
Calcifications and Ledges — Illumination and magnification using the DOM simplify identification and visualization of canal calcifications. A variety of chelating agents, ultrasonic instruments, rigid hand files or Mueller-type burs (e.g., Munce Discovery burs) can be used to eliminate calcified tissue and gain access to the canal. Clinicians can use the DOM, microexplorers and stiff, small-diameter hand files — along with lubricants and chelating agents — to carefully negotiate the canal. With a combination of hand files, Gates-Glidden drills or nickel-titanium rotary file systems, the canal is enlarged using the crown-down technique.10,24 Nonnegotiable calcified canals associated with periapical disease will require surgical intervention or extraction, if surgical treatment is contraindicated.
Iatrogenic ledges are produced when canal curvature is not maintained during cleaning and shaping.32 These complications can be reduced, however, by using nickel-titanium rotary instruments that tend to stay centered during canal preparation.33 After removing obstructions and filling materials, the ledge is visualized with the DOM. A Hedstrom, K or C file (that is curved at the file tip) is directed apically in order to bypass the ledge, which can be filed circumferentially with incrementally larger files until it is removed. If the ledge cannot be removed or bypassed, surgical treatment or extraction may be necessary when periapical pathosis is present.
Retrieving Separated Instruments — Various factors affect the removal of separated instruments, including the fragment’s size, length and location.10,24,34 Easily accessible fragments in the coronal portion of the canal system can be bypassed or ground away using burs or ultrasonics, while fragments located more apically (Figures 3A through 3H) may require the use of special devices (e.g., a Terauchi File Retrieval Kit or IRS Instrument Removal System).9,18,34 Longer fragments can often be retrieved using the braided technique by wrapping and twisting several Hedstrom or K files around the segment and directing energy coronally.9,18,24,35
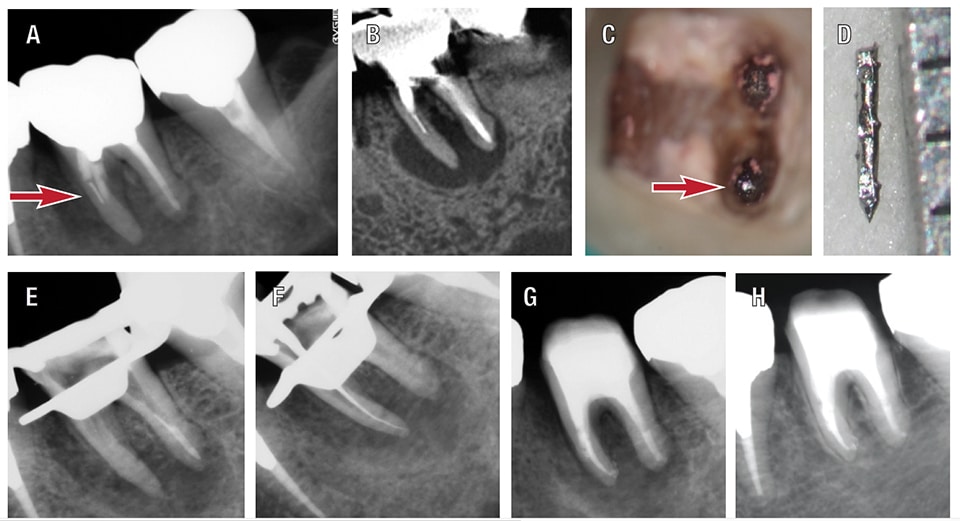
Removal success increases when the fragment is positioned coronal to the curvature. The energy of the ultrasonic tip must be directed to the inside portion of the canal curvature, carefully removing the tooth structure.34 Fragments located beyond the curvature and view of the DOM are unlikely to be removed and bypassed, thus, a surgical approach is indicated.24,36,37 Modified Gates-Glidden drills, ultrasonics, hand files or Mueller-type burs are used to gain access and generate a staging platform. This allows access to the coronal portion of the segment when the separated instrument is firmly embedded in the straight portion of the canal.10,36–41
Troughing and creating space around the top of the fragment and inside curve can be completed using small ultrasonic tips until the segment becomes loose in the canal, at which point it can be removed with the braided file technique, fragment removal kits using micro-lassos, soft metal microtubes matched with cyanocrylate glues, microtubes with lock wires, or ultrasonic tips set on high energy directed to the top of the segment.10,24,35,39,42 If the fragment is successfully removed, the apical canal can be cleaned and prepared with hand or rotary instruments. If the fragment is bypassed, however, the preparation is completed with hand instruments (because rotary instruments will tend to bind to the fragment, resulting in file fracture and separation). Moreover, if the fragment is unremovable, the presence of fractured instruments in the canal system will not necessarily prevent successful periapical healing.43,44
Gutta-Percha Removal — Gutta-percha can be removed with rotary or hand instruments, ultrasonics, solvents, heat systems or a combination of these approaches. When gutta-percha is poorly sealed and radiographic voids are visible, Gates-Glidden drills, hand reamers or Hedstrom files are effective for removal.39,45 If space exists or can be generated between the canal wall and obturation material, a Hedstrom file or hand reamer can be twisted in a clockwise direction to engage the gutta-percha; typically, the material can be removed in one piece when force is directed coronally. A crown-down technique prevents pushing debris apically into the periradicular tissues. After canal preparation with irrigants, inspection with the DOM will ensure that no gutta-percha or debris remain on canal walls.
Thermostatically heated hand pluggers and ultrasonic tips can be used to soften more densely packed gutta-percha. However, both techniques can be time consuming and are not always successful.39,45,46 An efficient method for removing gutta-percha employs a combination of Gates-Glidden drills and rotary files.45,47 Because gutta-percha can be extruded into the periapical tissues if too much force is applied, caution is advised — particularly when apical root resorption is present.48,49 Various types of rotary files have been specifically designed for gutta-percha removal; examples include the K3, ProTaper, GPX, R-Endo, Liberator, MTwo, Reciproc, EdgeFile XR and RaCe files.
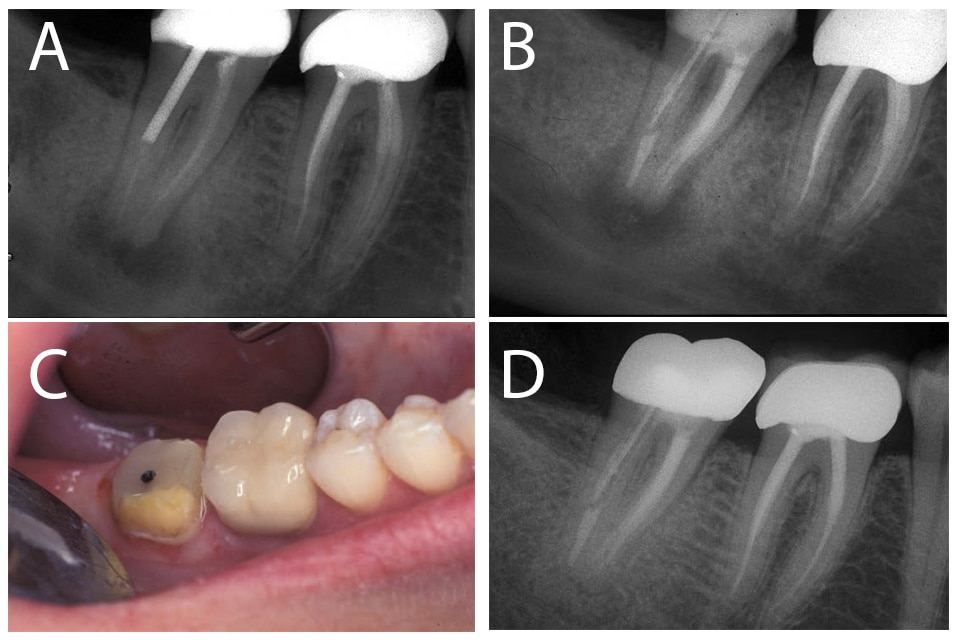
After removing obstructions and identifying the canals, the files are directed apically to remove gutta-percha in a coronal direction. This is an efficient technique in the straight and curved portions of canals, and is also effective when removing more recently developed obturation materials, including silicone-based methacrylate, glass ionomer, synthetic polymers and epoxy-based materials.50–54 However, removal of obturations with MTA-based sealers remains challenging because of their inherent physical properties (Figures 4A through 4D).55
Solvents — Although a variety of solvents will expedite gutta-percha removal, their use may leave residual gutta-percha and sealer on canal walls. When using solvents, small amounts are left in contact with the gutta-percha until it softens, at which point the material is removed with rotary or hand files. The most efficient solvents are chloroform, halothane and methylchloroform, but care is needed to ensure solvent is not extruded out the apical foramen.39,47,56–58
Silver Cones — After cement or core removal, retaining the coronal portion of a silver point is key to successfully retrieving silver cones.18 Utilizing magnification and illumination via the DOM is paramount when using ultrasonic tips or burs to produce space adjacent to the exposed silver point.59,60 Once the surrounding cement is removed with files and solvents, the point can be removed with the braided technique or various devices, such as Steiglitz forceps or modified microhemostats. An alternative method is to use soft metal tube extractors paired with cyanoacrylate glue or specialized kits.24,39,60–62
Carrier-Based Obturators — Whether fabricated from metal or plastic, carrier-based obturation systems can be removed using methods suitable for removing silver points, posts and gutta-percha. A pathway is generated that allows an instrument to engage the carrier once the gutta-percha has been softened with a solvent or heat source.63–68 Solvents can be used with heated pluggers or thermostatically controlled devices,67 but operators should avoid long periods of contact between dentin walls and heated tips, so as not to damage the surrounding bone and periodontium.68 The braided technique (used with multiple files) can grasp and remove plastic carriers after a pathway has been created with hand files or rotary instruments. Metal carriers are more effectively removed with ultrasonics, pliers, tapping devices or modified hemostats.63,65–67
Soft or Hard Pastes — Soft filling materials can generally be removed with hand or rotary instruments, using copious irrigation in a crown-down preparation.39 This will prevent extruding contaminated materials into the periapical tissues, and minimize the potential for posttreatment flare-ups. By comparison, hard pastes are typically more challenging to remove — and, in some cases, materials such as resorcinol-formalin paste (“Russian Red”) may be impossible to remove. Although manufacturers offer files with tempered points that can penetrate these materials initially, transportation and perforation are potential drawbacks in curved canals.18,39 The most predictable method for removing hard pastes remains ultrasonic instrumentation, paired with solvents. If there is a high probability that iatrogenic errors may occur during the process, periradicular surgical treatment should be considered.
REPAIRING PERFORATIONS
Perforations are pathologic or iatrogenic communications between the canal system and periodontium that can occur during retreatment; they can also be generated during the initial root canal procedure or by inflammatory resorption.69 Internal repair of previous iatrogenic perforations must be completed to ensure tooth retention. The prognosis depends on perforation location, size, and the time since the injury occurred.70 Paired with DOM visualization, the introduction of bioceramic or calcium-silicate-based cements (CSC) has significantly improved healing rates for perforations characterized by intact surrounding bone.71,72 A sampling of CSC products include ProRoot MTA, Endosequence Root Repair Material, Biodentine, Bioaggregate, MTA-Angelus and RetroMTA.73
POSTTREATMENT COMPLICATIONS
Flare-ups occur at a higher frequently in retreatment than initial root canal therapy.74–76 Thus, techniques for obturation material removal should be specifically selected to minimize the extrusion of debris and microorganisms into periradicular tissues.6 The use of rotary systems, side-venting needles and the crown-down technique — coupled with frequent irrigation — encourages debris removal in a coronal direction and minimizes material extrusion. Outcomes improve when employing dental dam isolation, evacuation systems, ultrasonic irrigation, calcium hydroxide dressing and canal inspection with the DOM to confirm all visible materials are cleared prior to obturation.6,26 In addition, a two-visit treatment approach decreases the probability of flare-ups associated with bacterial colonization, material contamination and preexisting periradicular disease.
FINAL CORONAL RESTORATION
Successful outcomes in endodontic retreatment hinge on the same restorative provision required for teeth receiving initial root canal therapy. Clinicians should avoid long-term provisional placement by providing a sealed final restoration in a timely manner, as this will prevent coronal microleakage and propagation of preexisting coronal infractions (when detectable). Restoration also conserves tooth structure and averts future revisions or surgical intervention.11,77
Recall visits are essential to monitor resolution of symptoms and evaluate periradicular healing or reemergence of posttreatment disease. Follow-up visits at six and 12 months are recommended to assess percussion and palpation testing. Mobility and periodontal probings should also be evaluated. Combined with radiographic imaging, this allows clinicians to monitor resolution (or nonresolution) of periapical pathosis. Recalls can also identify recurrent caries, restoration failures and other potential conditions.
To summarize, advances in instrumentation, irrigation systems, bioactive materials and the DOM have increased success rates in nonsurgical retreatment.78,79 It has been demonstrated that nonsurgical revision offers long-term outcomes superior to endodontic surgery; moreover, the success rate for surgical endodontics improves when combined with retreatment procedures.19,80 These advanced technologies and techniques have increased tooth survival rates and improved the quality of life for patients who wish retain their natural dentition.
References
- Davalou S, Gutmann JL, Nunn MH. Assessment of apical and coronal root canal seals using contemporary endodontic obturation and restorative materials and techniques. Int Endod J. 1999;32:388–396.
- Alley BS, Kitchens GG, Alley LW, Eleazer PD. A comparison of survival of teeth following endodontic treatment performed by general dentists or by specialists. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:115–118.
- Salehrabi R, Rotstein I. Epidemiologic evaluation of the outcomes of orthograde endodontic retreatment. J Endod. 2010;36:790–792.
- Molander A, Reit C, Dahlén G, Kvist T. Microbiological status of root-filled teeth with apical periodontitis. Int Endod J. 1998;31:1–7.
- Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative retreatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:86–93.
- Siqueira JF Jr. Microbial causes of endodontic flare-ups. Int Endod J. 2003;36:453–463.
- Allen RK, Newton CW, Brown CE, Jr. A statistical analysis of surgical and nonsurgical endodontic retreatment cases, J Endod. 1989;15:261-266.
- Hoen MM, Pink FE. Contemporary endodontic retreatments: an analysis based on clinical treatment findings. J Endod. 2002;28:834–836.
- Friedman S, Stabholz A. Endodontic retreatment — case selection and technique. Part 1: Criteria for case selection. J Endod. 1986;12:28–33.
- Ruddle CJ. Nonsurgical retreatment. J Endod. 2004;30:827–845.
- Saunders WP, Saunders EM. Coronal leakage as a cause of failure in root-canal therapy: a review. Endod Dent Traumatol. 1994;10:105–108.
- Ricucci D, Siqueira JF Jr. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010;36:1277–1288.
- Bogen G, Handysides R. Retreatment. In: Torabinejad M, Walton RE, Fouad AF. Endodontics Principles and Practice. 5th ed. St. Louis, Mo: Elsevier Saunders; 2015:355.
- Begotka BA, Hartwell GR. The importance of the coronal seal following root canal treatment. Va Dent J. 1996;73:8–10.
- Hartwell GR, Loucks CA, Reavley BA. Bacterial leakage of provisional restorative materials used in endodontics. Quintessence Int. 2010;41:335–339.
- Patel S, Durack C, Abella F, Shemesh H, Roig M, Lemberg K. Cone beam computed tomography in Endodontics — a review. Int Endod J. 2015;48:3–15.
- Yılmaz F, Kamburoglu K, Yeta NY, Oztan MD. Cone beam computed tomography aided diagnosis and treatment of endodontic cases: critical analysis. World J Radiol. 2016;8:716–725.
- Stabholz A, Friedman S: Endodontic retreatment — case selection and technique.Part 2: Treatment planning for retreatment. J Endod. 1988;14:607–614.
- Taschieri S, Machtou P, Rosano G, Weinstein T, Del Fabbro M. The influence of previous nonsurgical retreatment on the outcome of endodontic surgery. Minerva Stomatol. 2010;59:625–632.
- Wu D, Shi W, Wu J, Wu Y, Liu W, Zhu Q. The clinical treatment of complicated root canal therapy with the aid of a dental operating microscope. Int Dent J. 2011;61:261–266.
- Tsesis I, Faivishevsky V, Kfir A, Rosen E. Outcome of surgical endodontic treatment performed by a modern technique: a meta-analysis of literature. J Endod. 2009;35:1505–1511.
- von Arx T, Hänni S, Jensen SS. Correlation of bone defect dimensions with healing outcome one year after apical surgery. J Endod. 2007;33:1044–1048.
- Bogen G, Kuttler S. Mineral trioxide aggregate obturation: a review and case series. J Endod. 2009;35:777–790.
- Hülsmann M. Methods for removing metal obstructions from the root canal. Endod Dent Traumatol. 1993;9:223–237.
- Selbst AG. Understanding informed consent and its relationship to the incidence of adverse treatment events in conventional endodontic therapy. J Endod. 1990;16:387–390.
- Plotino G, Pameijer CH, Grande NM, Somma F. Ultrasonics in endodontics: a review of the literature. J Endod. 2007;33:81–95.
- Machtou P, Friedman S. Advances in endodontic retreatment. Alpha Omegan. 1997;90:47–55.
- Dixon EB, Kaczkowski PJ, Nicholls JI, Harrington GW. Comparison of two ultrasonic instruments for post removal. J Endod. 2002;28:111–115.
- Dominici JT, Clark S, Scheetz J, Eleazer PD. Analysis of heat generation using ultrasonic vibration for post removal. J Endod. 005;31:301–303.
- Altshul JH, Marshall G, Morgan LA, Baumgartner JC. Comparison of dentinal crack incidence and of post removal time resulting from post removal by ultrasonic or mechanical force. J Endod. 1997;23:683–686.
- Abbott PV. Incidence of root fractures and methods used for post removal. Int Endod J. 2002;35:63–67.
- Jafarzadeh H, Abbott PV. Ledge formation: review of a great challenge in endodontics. J Endod. 2007;33:1155–1162.
- Song YL, Bian Z, Fan B, Fan MW, Gutmann JL, Peng B. A comparison of instrument-centering ability within the root canal for three contemporary instrumentation techniques. Int Endod J. 2004;37:265–271.
- Terauchi Y, O’Leary L, Kikuchi I, et al. Evaluation of the efficiency of a new file removal system in comparison with two conventional systems. J Endod. 2007;33:585–588.
- Roig-Greene JL. The retrieval of foreign objects from root canals: a simple aid. J Endod. 1983;9:394–397.
- Iqbal MK, Rafailov H, Kratchman SI, Karabucak B. A comparison of three methods for preparing centered platforms around separated instruments in curved canals. J Endod. 2006;32:48–51.
- Gencoglu N, Helvacioglu D. Comparison of the different techniques to remove fractured endodontic instruments from root canal systems. Eur J Dent. 2009;3:90–95.
- Hülsmann M, Schinkel I. Influence of several factors on the success or failure of removal of fractured instruments from the root canal. Endod Dent Traumatol. 1999;15:252–258.
- Friedman S, Stabholz A, Tamse A. Endodontic retreatment — case selection and technique. 3. Retreatment techniques. J Endod. 1990;16:543–549.
- Souter NJ, Messer HH. Complications associated with fractured file removal using an ultrasonic technique. J Endod. 2005;31:450–452.
- Nehme W. A new approach for the retrieval of broken instruments. J Endod. 1999;25:633-635.
- Terauchi Y. Separated file removal. Dentistry Today. 2012;31:108,110-113. Available at dentistrytoday.com/endodontics/7322-separated-file-removal. Accessed March 6, 2017.
- Panitvisai P, Parunnit P, Sathorn C, Messer HH. Impact of a retained instrument on treatment outcome: a systematic review and meta-analysis. J Endod. 2010;36:775–780.
- Spili P, Parashos P, Messer HH. The impact of instrument fracture on outcome of endodontic treatment. J Endod. 2005;31:845–850.
- Hülsmann M, Stotz S. Efficacy, cleaning ability and safety of different devices for gutta-percha removal in root canal retreatment. Int Endod J. 1997;30:227–233.
- Wilcox LR, Krell KV, Madison S, Rittman B. Endodontic retreatment: evaluation of gutta-percha and sealer removal and canal reinstrumentation. J Endod. 1987;13:453–457.
- Ferreira JJ, Rhodes JS, Ford TR. The efficacy of gutta-percha removal using ProFiles. Int Endod J. 2001;34:267–274.
- Laux M, Abbott PV, Pajarola G, Nair PN. Apical inflammatory root resorption: acorrelative radio-graphic and histological assessment. Int Endod J. 2000;33:483–493.
- Vier FV, Figueiredo JA. Prevalence of different periapical lesions associated with human teeth and their correlation with the presence and extension of apical external root resorption. Int Endod J. 2002;35:710–719.
- Schirrmeister JF, Meyer KM, Hermanns P, Altenburger MJ, Wrbas KT. Effectiveness of hand and rotary instrumentation for removing a new synthetic polymer-based root canal obturation material (Epiphany) during retreatment. Int Endod J. 2006;39:150–156.
- Ezzie E, Fleury A, Solomon E, Spears R, HE J. Efficacy of retreatment techniques for a resin-based root canal obturation material. J Endod. 2006;32:341–344.
- de Oliveira DP, Barbizam JV, Trope M, Teixeira FB: Comparison between gutta-percha and resilon removal using two different techniques in endodontic retreatment. J Endod. 2006;32:362–364.
- Roberts S, Kim JR, Gu LS, et al. The efficacy of different sealer removal protocols on bonding of self-etching adhesives to AH plus-contaminated dentin. J Endod. 2009;35:563–567.
- Kuga MC, Faria G, Rossi MA, et al. Persistence of epoxy-based sealer residues in dentin treated with different chemical removal protocols. Scanning. 2013;35:17–21.
- Neelakantan P, Grotra D, Sharma S. Retreatability of 2 mineral trioxide aggregate-based root canal sealers: a cone-beam computed tomography analysis. J Endod. 2013;39:893–896.
- Horvath SD, Altenburger MJ, Naumann M, Wolkewitz M, Schirrmeister JF. Cleanliness of dentinal tubules following gutta-percha removal with and without solvents: a scanning electron microscopic study. Int Endod J. 2009;42:1032–1038.
- Chutich MJ, Kaminski EJ, Miller DA, Lautenschlager EP. Risk assessment of the toxicity of solvents of gutta-percha used in endodontic retreatment. J Endod. 1998;24:21–216.
- Hansen MG. Relative efficiency of solvents used in endodontics. J Endod. 1998;24:38–40.
- Plack WF 3rd, Vire DE. Retrieval of endodontic silver points. Gen Dent. 1984;32:124–127.
- Suter B. A new method for retrieving silver points and separated instruments from root canals. J Endod. 1998;24:446–448.
- Kvist T, Reit C. Results of endodontic retreatment: a randomized clinical study comparing surgical and nonsurgical procedures. J Endod.1999;25:814–817.
- Spriggs K, Gettleman B, Messer HH. Evaluation of a new method for silver point removal. J Endod. 1990;16:335–338.
- Ibarrola JL, Knowles KI, Ludlow MO. Retrievability of Thermafil plastic cores using organic solvents. J Endod. 1993;19:417–418.
- Wilcox LR. Thermafil retreatment with and without chloroform solvent. J Endod. 1993;19:563–566.
- Imura N, Zuolo ML, Kherlakian D. Comparison of endodontic retreatment of laterally condensed gutta-percha and Thermafil with plastic carriers. J Endod. 1993;19:609–612.
- Zuolo ML, Imura N, Ferreira MO. Endodontic retreatment of Thermafil or lateral condensation obturations in post space prepared teeth. J Endod. 1994;20:9–12.
- Wolcott JF, Himel VT, Hicks ML. Thermafil retreatment using a new “System B” technique or a solvent. J Endod. 1999;25:761–764.
- Lipski M, Wozniak K. In vitro infrared thermographic assessment of root surface temperature rises during Thermafil retreatment using system B. J Endod. 2003;29:413–415.
- Bogen G, Munce JC, Chandler N. Repair of perforations in endodontically treated Teeth. In: Baba NZ, ed. Contemporary Restoration of Endodontically Treated Teeth. Hanover Park, Il: Quintessence Publishing Co Inc; 2012:167.
- Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol. 1996;12:255–264.
- Pace R, Giuliani V, Pagavino G. Mineral trioxide aggregate as repair material for furcal perforation: case series. J Endod. 2008;34:1130–1133.
- Mente J, Hage N, Pfefferle T, et al. Treatment outcome of mineral trioxide aggregate: repair of root perforations. J Endod. 2010;36:208–213.
- Cao Y, Bogen G, Lim J, Shon WJ, Kang MK. Bioceramic materials and the changing concepts in vital pulp therapy. J Calif Dent Assoc. 2016;44:279–290.
- Torabinejad M, Kettering JD, McGraw JC, Cummings RR, Dwyer TG, Tobias TS. Factors associated with endodontic interappointment emergencies of teeth with necrotic pulps. J Endod. 1988;14:261–266.
- Trope M. Flare-up rate of single-visit endodontics. Int Endod J. 1991;24:24–26.
- Walton R, Fouad A. Endodontic interappointment flare-ups: a prospective study of incidence and related factors. J Endod. 1992;18:172–177.
- Paik S, Sechrist C, Torabinejad M. Levels of evidence for the outcome of endodontic retreatment. J Endod. 2004;30:745–750.
- Gillen BM, Looney SW, Gu LS, et al. Impact of the quality of coronal restoration versus the quality of root canal fillings on success of root canal treatment: a systematic review and meta-analysis. J Endod. 2011;37:895–902.
- He J, White RK, White CA, Schweitzer JL, Woodsmansey KF. Clinical and patient-centered outcomes of nonsurgical root canal retreatment in first molars using contemporary techniques. J Endod. 2017;43:231–237.
- Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009;35:930–937.
Featured photo by iStock_Oles/iStock / getty images plus
From Decisions in Dentistry. April 2017; 3(4):37–42.




