CE Sponsored by Colgate in Partnership With the American Academy of Periodontology: Overview of the New Peri-implant and Periodontal Disease Classification System
Reflecting the latest scientific insights, the newly updated periodontal disease classification system includes the inaugural classifications for peri-implant conditions.
This course was published in the October 2018 issue and expires October 2021. The author has no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
EDUCATONAL OBJECTIVES
After reading this course, the participant should be able to:
- Explain classification systems for periodontal and peri-implant diseases and conditions, as developed by the American Academy of Periodontology and European Federation of Periodontology.
- Describe factors that can lead to the development of periodontal and peri-implant diseases — and the clinical indications of such conditions.
- Discuss clinical considerations for diagnosing periodontal and peri-implant diseases.
Introduction
The 2018 classification system for periodontal and peri-implant diseases and conditions developed by the American Academy of Periodontology and European Federation of Periodontology represents an important collaborative effort that extensively surveyed the existing evidence, evaluated reviews, and reached consensus regarding the updated classifications. This exciting enhancement as to how these diseases are understood, communicated and treated advances the science behind disease diagnosis. It strives for greater diagnostic precision, and offers guidance for clinical application by introducing a multi-dimensional staging and grading system for periodontal disease, as well as the first classifications for peri-implant disease. Intended to improve clinicians’ understanding of disease progression and risk factors, the new system highlights the complex nature of the disease and need for individualized treatment. I hope you find this article a valuable resource and embrace the key points that differentiate the new classifications from the prior system. The Colgate-Palmolive Company is delighted to have provided an unrestricted educational grant to support the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions in Chicago in November 2017 and this continuing education article and series.
—Matilde Hernandez, DDS, MS, MBA
Scientific Affairs Manager Professional Oral Care
Colgate Oral Pharmaceuticals
This overview of the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions will help clinicians better understand the classifications and new staging and grading system
From the American Academy of Periodontology
This summer, the American Academy of Periodontology (AAP) was thrilled to release the proceedings from the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions. The landmark event, held last November in Chicago, welcomed some of the world’s foremost periodontal experts to deliberate and define what constitutes periodontal health and disease. Given the strides made in our understanding of disease progression, risk, and the individual considerations of each patient, this new system will help practitioners provide the highest standard of care.
In this article, educator and AAP periodontist Theodoros Katsaros, DDS, MSD, shares highlights from the new disease classification. We believe the new classification — which includes a multidimensional staging and grading system for periodontitis, as well as the inaugural classification for peri-implant diseases and conditions — will be a useful resource for clinicians everywhere. The AAP is proud to work with Decisions in Dentistry and Colgate-Palmolive as we fulfill our commitment to enhancing the successful practice and delivery of effective care.
—Steven R. Daniel, DDS
President, American Academy of Periodontology
As with any type of oral health care, the progression toward a correct diagnosis when providing periodontal therapy involves data collection and analysis from the clinical and radiographic examination, as well as the patient interview. A well-organized and complete periodontal disease classification system that is based on the most recent scientific knowledge is of great value at many levels. As one example, it will help improve communication with patients, peers and insurance carriers, which, in turn, supports high-quality care.
In November 2017, the World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions took place in Chicago. The workshop was a joint effort of the American Academy of Periodontology (AAP) and European Federation of Periodontology that involved more than 120 participants from around the world. The efforts of four workgroups, each focusing on different diseases and conditions, resulted in numerous publications, including 18 narrative or systematic reviews and four consensus reports. This article will present an overview of the new 2018 classification system. The major changes or additions to the previous periodontal disease classifications1 — published in 1999 — are highlighted. These include a staging and grading system for periodontitis, and the first-ever classifications for peri-implant conditions.
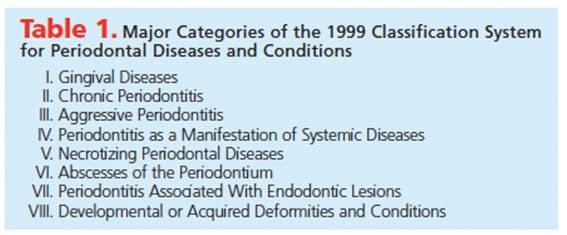
According to the previous classification system, periodontal diseases and conditions were classified under eight main categories (Table 1). Although widely used for nearly two decades, limitations were identified throughout this period. The diagnosis of periodontitis was initially based on clinical attachment levels. The calculation of attachment levels includes the identification of the position of the gingival margin in relation to the cemento-enamel junction (CEJ). This is an easy task in the presence of gingival recession; however, it is more challenging in cases in which the gingival margin is located in a more coronal position to that of the CEJ. This could result in inaccurate calculation of the attachment levels and, consequently, in over-diagnosis of periodontitis. To address these concerns, the AAP published an update in 2015 adding radiographic interproximal bone levels and probing depths as essential components in the diagnosis of periodontitis.2 In addition, although dental implants were introduced in North America in the early 1980s, when the 1999 classifications were published, their use was not as widespread as it is today. As a result, peri-implant diseases and conditions were not included in the previous classification system.
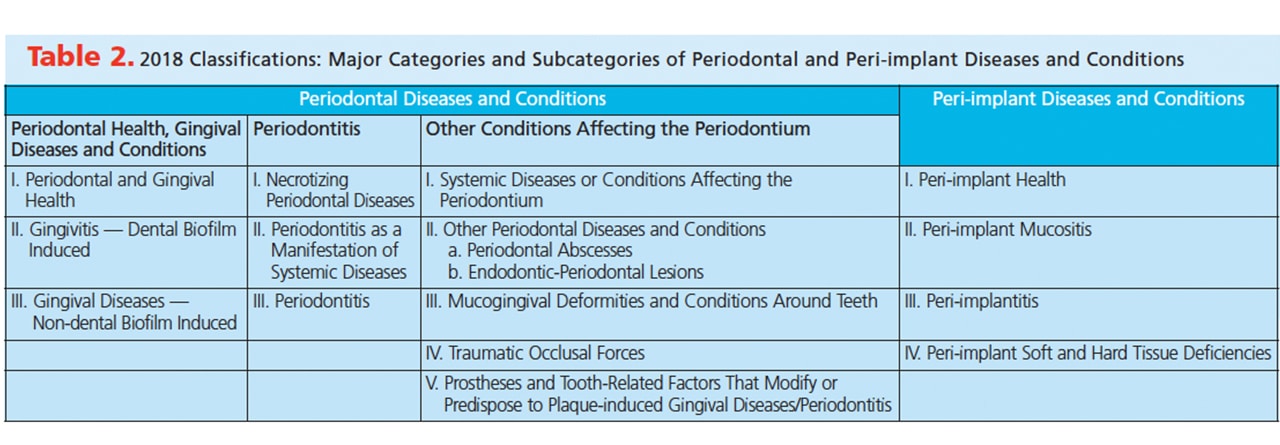
The 2018 classifications are organized in two main categories: (1) Periodontal Diseases and Conditions, which are further divided in three subcategories (gingival health/gingival diseases and conditions, periodontitis, and other conditions affecting the periodontium), and (2) Peri-implant Diseases and Conditions (Table 2).3
PERIODONTAL DISEASES AND CONDITIONS
Periodontal Health and Gingival Diseases and Conditions
I. Periodontal and Gingival Health: Periodontal health can be observed in both intact periodontium or reduced periodontium. A presentation of reduced periodontium can result from a history of periodontitis, recession, or following specific surgical interventions (such as crown lengthening). The workshop described four categories of health that reflect different clinical situations.4
- Pristine Gingival Health is characterized by no bleeding on probing (BOP) or attachment loss, probing depths less than 3 mm, and no clinical signs of inflammation.
- Clinically Healthy is the absence or low levels of signs of inflammation
- Periodontal Disease Stability is observed in cases of treated periodontitis in which the ideal outcomes are achieved (e.g., reduction of probing depth to 3 mm or less, control of all local and systemic factors involved, and complete resolution or minimal signs of clinical inflammation)
- Periodontal Disease Remission/Control represents a compromised scenario of gingival health. Following therapy, and despite some reduction in probing depths, control of local and systemic factors is not complete and resolution of the inflammation is not entirely achieved.
It should be noted that periodontal health is not only determined on the basis of clinical findings, such as probing depths and clinical attachment levels. Additional factors related to periodontal health should be taken into account, including microbiological determinants (plaque composition), host determinants (tooth anatomic factors and host status), and environmental determinants (such as smoking or stress).
II. Gingivitis — Dental Biofilm Induced: As part of the new periodontal disease classification system, the term “incipient gingivitis” was proposed. It is characterized by minimal BOP that is observed in less than 10% of sites. This condition is a variant of gingival health, but, if left untreated, can rapidly progress to gingivitis.
Dental biofilm-induced gingivitis represents a common disease entity. It can observed in patients with intact periodontium, as well as in individuals with reduced periodontium due to periodontitis or other reasons (e.g., recession or a history of crown lengthening surgery). Clinically, these patients will present with BOP in 10% or more of the sites, while the probing depths will be in the range of 1 mm to 3 mm. Attachment loss may or may not be present, depending on the patient’s periodontal history.5
Despite the fact bacterial plaque is the etiology of the disease, its clinical manifestation can vary based on a multitude of modifying factors that can contribute to either exacerbation or attenuation of the clinical signs of inflammation. Examples of exacerbating factors include puberty or pregnancy, while smoking is considered an attenuating factor. Accounting for these factors and controlling them, when possible, are both critical to the successful management of gingivitis. In order for the diagnosis of gingivitis to be more descriptive of the clinical findings, it can be classified as localized or generalized (if it includes less or more than 30% of the teeth, respectively), and its severity described as mild, moderate or severe.6
Under the new periodontal disease classification, drug-influenced gingival enlargement is a separate clinical entity and included as a modifying factor of biofilm-induced gingivitis. Due to the enlargement caused by specific medications (e.g., phenytoin, nifedipine or cyclosporine), oral hygiene becomes more challenging, eventually leading to increased plaque accumulation and more severe clinical inflammation.7
III. Gingival Diseases — Non-dental Biofilm Induced: This category includes, among others, a number of diseases and conditions of specific viral, fungal or bacterial origin, reactive process, and gingival pigmentation. Compared to the 1999 classification, a notable change is the removal of linear gingival erythema from the list, as it now considered a form of candidiasis. Additionally, ascorbic acid deficiency-associated gingivitis and similar forms of gingivitis (e.g., puberty-associated or menstrual cycle-associated) were eliminated.8
Periodontitis
I. Necrotizing Periodontal Diseases: Necrotizing gingivitis, necrotizing periodontitis and necrotizing stomatitis are listed in this category. The latter was added under the 2018 classification and is characterized by necrosis that extends beyond the mucogingival junction. It is commonly associated with severely immunocompromised patients. The term “ulcerative” is no longer included as part of these diagnoses because ulceration is considered to be secondary to necrosis. Necrotizing diseases are categorized on the basis of the patient’s immune status.9
II. Periodontitis as a Manifestation of Systemic Conditions: The specifics of this category will be discussed in an upcoming section (Systemic Diseases or Conditions Affecting the Periodontium), as it appears that some degree of overlap exists between these categories.
III. Periodontitis: The most significant changes in the new periodontal disease classification system are arguably found in this category. The terms “chronic” and “aggressive periodontitis” are eliminated and now described as periodontitis. Although there are phenotypic characteristics that differ between chronic and aggressive periodontitis, the rationale is that the pathophysiology of the two is the same. Additionally, there is significant heterogeneity to several aspects of the study designs investigating aggressive periodontitis. Overall, there is not enough evidence at this time to support the notion that aggressive periodontitis constitutes a separate clinical entity.10
Three steps are now required to properly diagnose periodontitis:
- Identification of attachment loss in more than two non-adjacent teeth; the attachment loss should be related only to periodontitis, and other potential etiologies (such as recession, root fracture and defective restorations) should be excluded
- Identification of the form of periodontitis (e.g., necrotizing, manifestation of systemic conditions, or periodontitis)
- Description of the presentation, based on the newly introduced staging and grading system11
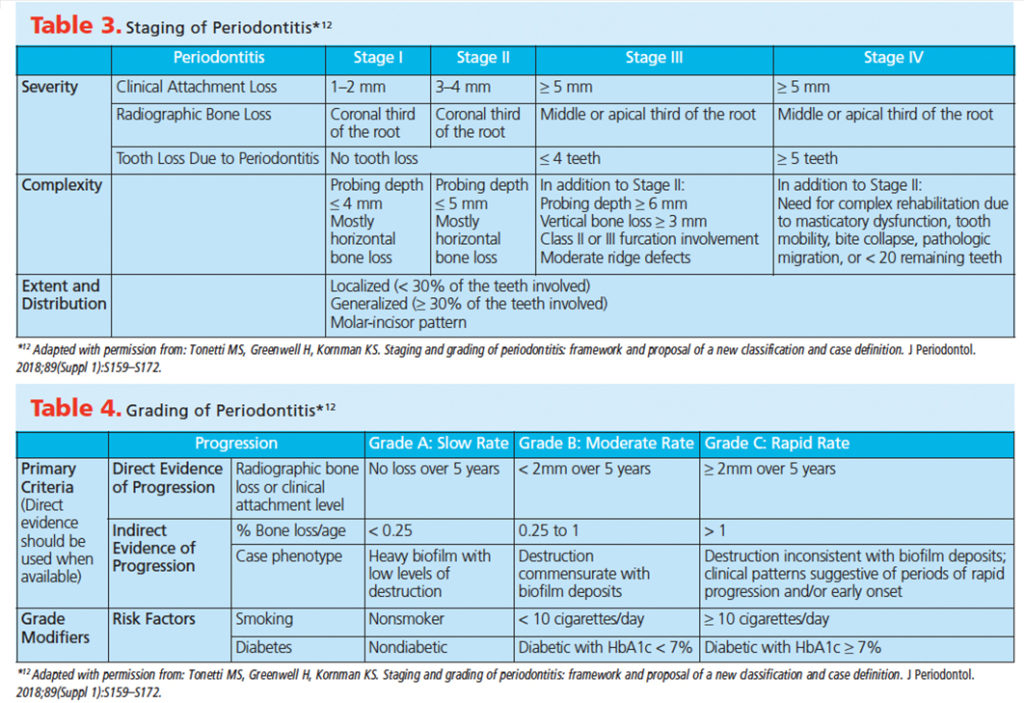
Besides clinical and radiographic findings (including attachment loss, radiographic bone loss and probing depths), the new staging system accounts for a multitude of factors that influence case management — such as teeth lost to periodontal disease, number of missing teeth, the presence of vertical bony defects, posterior bite collapse, and the extent and distribution of the disease. Following data collection from the patient’s medical/dental history and clinical and radiographic exam, periodontitis cases are categorized as stages I to IV, based primarily on attachment levels. A higher stage should be assigned if at least one of the criteria listed in the higher stage is identified. As a rule, cases of chronic periodontitis that were previously diagnosed as slight or localized moderate will be classified as Stage I, generalized moderate will be Stage II, and severe periodontitis cases will be classified as stages III or IV (Table 3).
Once the disease stage is determined, it is graded as A, B or C, based on the risk for future progression. Grading is affected by a combination of local and systemic factors, such as ratio of bone loss to age, amount of bacterial plaque deposits, smoking and diabetes (Table 4).12
Other Conditions Affecting the Periodontium
I. Systemic Diseases or Conditions Affecting the Periodontium: These diseases and conditions are associated with attachment and/or bone loss, and are classified in three subcategories. A number of systemic conditions are included in the first subcategory. The changes observed in the periodontium are not related to dental biofilm, but are secondary to the systemic condition already diagnosed, such as Down syndrome, Ehlers-Dahnlos syndromes types IV and VIII, or human immunodeficiency virus infection. The second subcategory is dedicated to systemic modifiers of periodontitis (e.g., smoking, obesity or osteoporosis), while the third category includes diseases that result in bone loss (irrespective of periodontitis), such as malignancies.13,14
II. Other Periodontal Diseases and Conditions: (A) Periodontal Abscesses: The former distinction between gingival and periodontal abscesses is no longer followed. Under the new periodontal disease classification, periodontal abscesses are classified on the basis of their etiology and the patient’s possible history of periodontitis. The pericoronal abscess that was associated with semi-impacted teeth is also eliminated, as it was considered non-relevant, despite the fact that it can, indeed, be an acute condition.
(B) Endodontic-Periodontal Lesions: In the past, combined endodontic-periodontal lesions were classified according to the primary lesion (e.g., primary endodontic with secondary periodontal). The similarities in the microbial profile and challenges associated with identifying the primary lesion were two of the reasons that led to the new classification, which is based on clinical findings, signs and symptoms.9
III. Mucogingival Deformities and Conditions Around Teeth: The periodontal biotype and its classification as thin scalloped, thick scalloped or thick flat were added in this category. Another change from 1999 is classification of gingival recession based on severity. A table encompassing some of the aspects affecting the therapeutic outcome — such as gingival thickness, keratinized tissue width, the presence or absence of noncarious cervical lesions, and a detectable cemento-enamel junction — was also proposed as part of the new system.13,15
IV. Traumatic Occlusal Forces: This term replaced the previously used excessive occlusal forces. Occlusal forces are described as traumatic if they cause trauma in the periodontal tissues and/or occlusal wear of the teeth. Occlusal trauma can still be classified as primary or secondary, while the addition of orthodontic forces under this category is also noteworthy.16
V. Prostheses and Tooth-Related Factors That Modify or Predispose to Plaque-induced Gingival Diseases/Periodontitis: Root fractures, root proximity, tooth anatomical considerations, hypersensitivity, and clinical procedures related to the fabrication of restorations are among the factors included in this category. Altered passive eruption, a condition that was absent from the 1999 classification, is also included as a tooth-related factor. The negative effect of the restoration margins when placed within the supracrestal tissue attachment (formerly known as biologic width), and the increase of mobility of teeth used as abutments in distal extension removable dental partials are highlighted.17
PERI-IMPLANT DISEASES AND CONDITIONS
I. Peri-implant Health: Compared to periodontal tissues, it is more challenging to define what is considered “physiologic” in regard to peri-implant tissues. In general, probing depths should be 5 mm or less, crestal bone remodeling following delivery of the prosthesis should be no more than 2 mm, and there should be an absence of clinical signs of inflammation (Table 5).18,19
II. Peri-implant Mucositis: Peri-implant mucositis is a disease of bacterial etiology, with similar characteristics to gingivitis. However, peri-implant mucositis requires longer time to resolve (approximately three weeks) after the etiology is addressed. Additionally, compared to natural teeth, bacterial plaque will result in more pronounced inflammatory response around implants.19,20
III. Peri-implantitis: This disease is plaque associated and characterized by inflammation of the peri-implant tissues and progressive bone loss around the implant. A history of periodontal disease is considered a risk factor for developing peri-implantitis, and any residual cement on an implant prosthesis is also a potential risk factor. Compliance with recommended periodontal maintenance intervals will reduce the risk for peri-implantitis.19,21,22
IV. Peri-implant Soft and Hard Tissue Deficiencies: These conditions are classified based on their occurrence before or after implant placement. Factors that can potentially affect hard and soft tissue deficiencies prior to implant placement include tooth loss, trauma from the extraction, infections and periodontitis. On the other hand, hard tissue deficiencies following implant placement may be affected by the positioning of the implant, peri-implantitis and soft tissue thickness (among other factors). Peri-implant soft tissue deficiencies following implant placement can be affected by the lack of buccal bone or interproximal bone, amount of keratinized tissue, and changes in the dento-alveolar complex that occur over time.22,23
CONCLUSION
The new peri-implant and periodontal disease classification addresses most of the limitations identified in the 1999 classification system. Implant dentistry is part of daily clinical practice, and the introduction of case definitions for peri-implant diseases and conditions was much needed.
The staging and grading of periodontitis is descriptive of not only the extent and severity of the disease, it is also suggestive of different aspects, such as the complexity of management, disease progression, and the patient’s systemic status. These factors are of great importance and were already taken into account when assigning a prognosis or during risk assessment. The prognosis represents a dynamic process that is continuously reassessed as new information is collected at each subsequent visit. By comparison, diagnosis typically precedes prognosis and is established during the initial visits. The collection of all the information required for the staging and grading of periodontitis can, in some circumstances, be a challenging task to complete within the first appointments. In light of these challenges, the ease of transition in implementing this new classification system in clinical practice is yet to be determined.
RECAP OF THE 2018 PERIODONTAL DISEASE CLASSIFICATION SYSTEM
The 2018 classification system for periodontal and peri-implant diseases and conditions developed by the American Academy of Periodontology and European Federation of Periodontology represents a sea-change from the previous 1999 classifications. Here is a recap of key points that differentiate the new classifications from the prior system.
PERIODONTAL DISEASES AND CONDITIONS
Periodontal Health and Gingival Diseases and Conditions Key Points: Specific criteria for gingival health are established under the new classification system. Gingival health, as well as gingivitis, can be observed in both intact and reduced periodontium. Localized, slight inflammation is compatible with health and, among other criteria, bleeding on probing (BOP) in 10% or more of the sites is required for the diagnosis of dental biofilm-induced gingivitis. Lower levels of BOP (< 10%) are considered a variant of health; in fact, the term “incipient gingivitis” was introduced to describe this clinical presentation.
Periodontitis Key Points: Necrotizing diseases are no longer characterized as ulcerative. It should be noted that necrotizing gingivitis is included in the periodontitis category, even though clinical findings associated with it are confined in the interproximal soft tissues, and there is no bone loss as a result of the disease.
Utilization of the system for staging and grading includes components of not only the diagnosis, but also the management and future progression of the disease. This is consistent with the goal of a more holistic approach to managing periodontal patients. The new classification emphasizes the potential link between periodontal status and systemic conditions. The grading system is designed in a dynamic way, and allows for updates and modifications in case relevant evidence emerges in the future. Although detailed criteria are provided for each stage and grade of periodontitis, clinical judgment is highly important in the correct diagnosis of the disease.
Other Conditions Affecting the Periodontium Key Points: Endodontic-periodontal lesions are no longer classified according to the primary lesions. There is no distinction between periodontal and gingival abscesses, as the diagnosis of periodontal abscesses includes both of the above. In addition to the diagnosis of gingival recession, its severity should also be described and included in a number of factors that will affect treatment decisions and outcomes.
Important changes in terminology are also included in the new classification system. Traumatic occlusal force replaces excessive occlusal force. Periodontal phenotype (associated with clinical characteristics) replaces periodontal biotype (associated with genetic characteristics). In addition, biologic width is now replaced by supracrestal tissue attachment (and still refers to the junctional epithelium and connective tissue attachment).
PERI-IMPLANT DISEASES AND CONDITIONS
Peri-implant Health, Peri-implant Mucositis and Peri-implantitis Key Points: The amount of crestal bone remodeling around implants, and, consequently, the stability of the soft and hard tissues, are affected by multiple factors. The design of the abutment and prosthesis, placement of the implant in relation to the implant crest, implant design, implant-abutment connection, surgical technique, and thickness of the soft tissues are only some of the factors influencing peri-implant diseases and conditions. It is therefore critical for an accurate diagnosis and a baseline of the clinical and radiographic characteristics to be established, as this will allow for longitudinal monitoring of these characteristics and identification of possible alterations.
For these reasons, a clinical and radiographic exam is recommended within the first year of prosthesis delivery. In the event these data are not available, different criteria apply for the definition of peri-implantitis.22 An overview of the case definitions of peri-implant health, peri-implant mucositis and peri-implantitis is presented in Table 5.
REFERENCES
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999;4:1–6.
- American Academy of Periodontology Task Force report on the update to the 1999 classification of periodontal diseases and conditions. J Periodontol. 2015;86:835–838.
- Caton J, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant diseases and conditions — introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1–S8.
- Lang NP, Bartold PM. Periodontal health. J Periodontol. 2018;89(Suppl 1):S9–S16.
- Trombelli L, Farina R, Silva CO, Tatakis DN. Plaque-induced gingivitis: case definition and diagnostic considerations. J Clin Periodontol. 2018;45(Suppl 20):S44–S67.
- Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38:610–616.
- Murakami S, Mealey BL, Mariotti A, Chapple IL. Dental plaque–induced gingival conditions. J Periodontol. 2018;89(Suppl 1):S17–S27.
- Holmstrup P, Plemons J, Meyle J. Non–plaque-induced gingival diseases. J Periodontol. 2018;89(Suppl 1):S28–S45.
- Herrera D, Retamal-Valdes B, Alonso B, Feres M. Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endo-periodontal lesions. J Periodontol. 2018;89(Suppl 1):S85–S102.
- Fine DH, Patil AG, Loos BG. Classification and diagnosis of aggressive periodontitis. J Periodontol. 2018;89(Suppl 1):S103–S119.
- Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–S182.
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: framework and proposal of a new classification and case definition. J Periodontol. 2018;89(Suppl 1):S159–S172.
- Jepsen S, Caton JG, Albandar JM, et al. Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S237–S248.
- Albandar JM, Susin C, Hughes FJ. Manifestations of systemic diseases and conditions that affect the periodontal attachment apparatus: case definitions and diagnostic considerations. J Clin Periodontol. 2018;45(Suppl 20):S171–S189.
- Cortellini P, Bissada NF. Mucogingival conditions in the natural dentition: narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S204–S213.
- Fan J, Caton JG. Occlusal trauma and excessive occlusal forces: narrative review, case definitions, and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S214–S222.
- Ercoli C, Caton JG. Dental prostheses and tooth-related factors. J Periodontol. 2018;89(Suppl 1):S223–S236.
- Araujo MG, Lindhe J. Peri-implant health. J Periodontol. 2018;89(Suppl 1):S249–S256.
- Renvert S, Persson GR, Pirih FQ, Camargo PM. Peri-implant health, peri-implant mucositis, and peri-implantitis: case definitions and diagnostic considerations. J Periodontol. 2018;89(Suppl 1):S304–S312.
- Heitz-Mayfield LJ, Salvi GE. Peri-implant mucositis. J Periodontol. 2018;89(Suppl 1):S257–S266.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol. 2018;89(Suppl 1):S267–S290.
- Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S313–S318.
- Hämmerle CH, Tarnow D. The etiology of hard and soft-tissue deficiencies at dental implants: a narrative review. J Periodontol. 2018;89(Suppl 1):S291–S303.
Featured image by FILADENDRON/E+//ISTOCK/GETTY IMAGES PLUS
From Decisions in Dentistry. October 2018;4(10)25–30.