Caring for Patients With Attention-Deficit/Hyperactivity Disorder
These clinical tips will assist dental teams in treating this patient population.
PURCHASE COURSE
This course was published in the May issue and expires May 2020. The authors have no commercial conflicts of interest to disclose. This 2 credit hour self-study activity is electronically mediated.
OBJECTIVES
After reading this course, the participant should be able to:
- Define the subtypes and classification of attention deficit/hyperactivity disorder (ADHD).
- Discuss the prevalence and etiology of this condition.
- List the comorbidities, oral health risks and treatments associated with ADHD.
- Identify strategies for providing oral health care to these patients.
One of the most common childhood disorders, attention-deficit/hyperactivity disorder (ADHD) affects approximately 11% of children.1 Although symptoms persist into adolescence and adulthood in the majority of cases,2 individuals with ADHD can be treated successfully in the general dental practice, regardless of age. In order to provide effective care, dental professionals need to understand the condition’s symptoms, offer scheduling modifications, provide clear and consistent communication, and work in tandem with the family and other health care professionals.
This disorder is classified as a neurobehavioral syndrome. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), symptoms of ADHD include difficulty staying focused and paying attention, problems controlling behavior, and hyperactivity.3 At present, the most valid approach to determining the presence of ADHD is by collecting information through rating scales and diagnostic interviews with parents/caregivers and teachers about exhibited behaviors and associated impairment, as well as behavioral observations.4
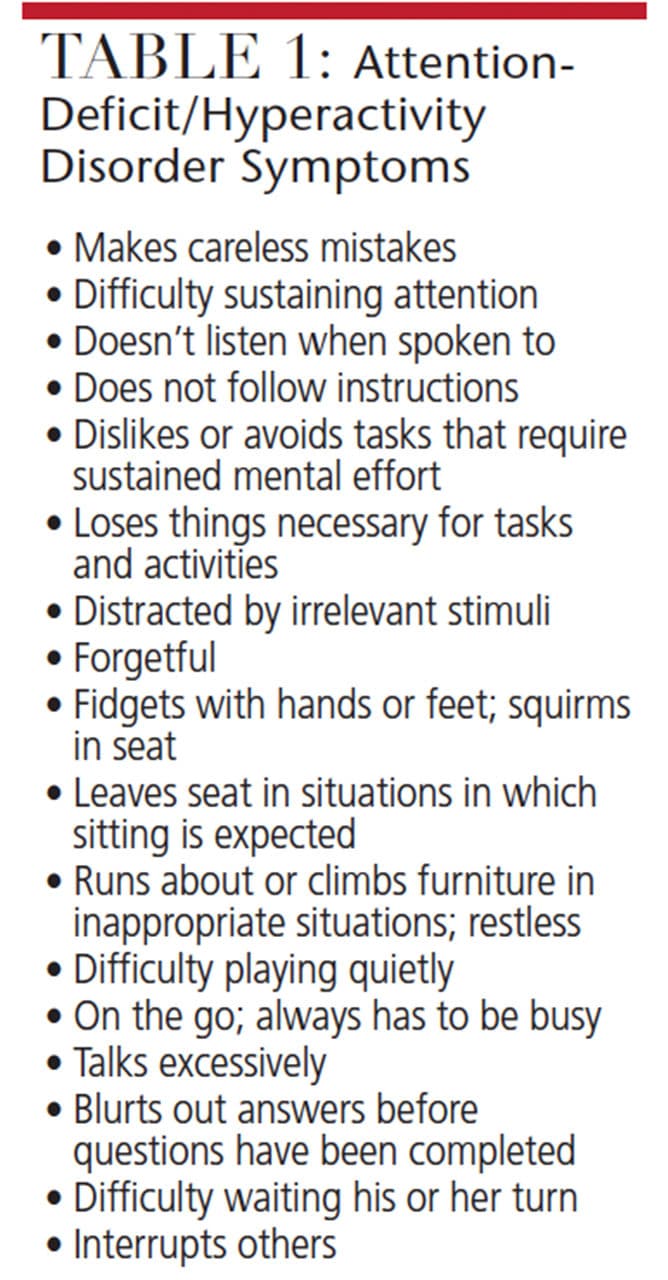
There are three subtypes of ADHD: predominantly hyperactive-impulsive, predominantly inattentive, and combined hyperactive-impulsive and inattentive (see Table 1 for list of symptoms).3 Children with more overt misbehaviors and externalizing psychopathology often prompt teachers to make referrals and parents/caregivers to seek mental health care.5,6 As a result, children with the predominantly inattentive subtype may be less likely to display obvious misbehavior compared to individuals with the hyperactive subtype, and are thus less likely to be referred for mental health services.
Deficits have been among the numerous causal factors, ADHD is extremely heritable, so genetics is likely a main contributor. If a parent is diagnosed with ADHD, there is a 57% chance that his or her child will have ADHD.7 About a third of siblings of a child with this condition will have a similar diagnosis.8 The identical twin of a child with ADHD has a 75% to 97% chance of also being diagnosed.9
There are also neurological contributing factors. Deficits have been identified in children with ADHD in their frontal lobe, the area of the brain responsible for executive functions (such as impulse/emotional control, working memory, planning/prioritizing and organization).9 It is also thought to be caused by problems in the regulation of two neurotransmitters (dopamine and norepinephine), which affect the ability to focus on tasks.9
Like many other illnesses, ADHD probably results from a combination of factors. In addition to genetics and neurobiological factors, for example, its etiology may include prenatal exposure to tobacco use, lead, alcohol, cocaine, pregnancy or birth complications, and brain injury/infections may also play a role.9
PREVALENCE
In 2011, approximately 6.4 million children ages 4 to 17 years (11%) had been clinically diagnosed with ADHD,10 ranging from 2.7% for those ages 4 to 5 years, 9.5% for 6- to 11-year-olds, and 11.8% for 12- to 17-year-olds. Among all age groups, prevalence of having been diagnosed with ADHD was more than twice as high for boys than girls. Symptoms persist into adulthood in 50% of youth with ADHD.2
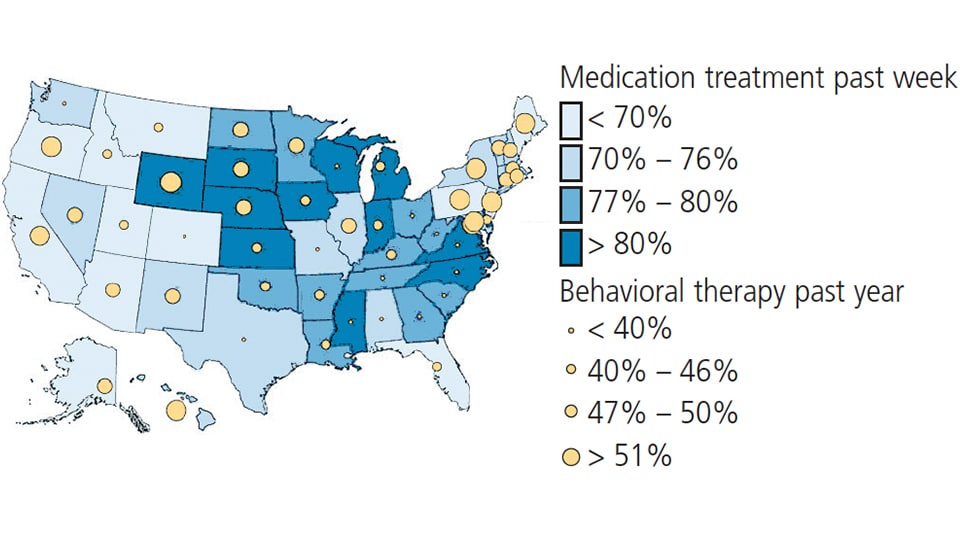
Prevalence varies substantially by state, ranging from a low of 4.2% in Nevada to a high of 14.8% in Kentucky (Figure 1).11 There are also marked differences by state in the proportion of children receiving services to treat ADHD. For example, the percentage of youth diagnosed with ADHD that reported receiving medication ranged from 3.2% in Hawaii to 10.4% in Louisiana. Similarly, there are marked differences in the proportion receiving behavioral therapy, ranging from 32.5% in Tennessee to 60.6% in Hawaii (Figure 2).10
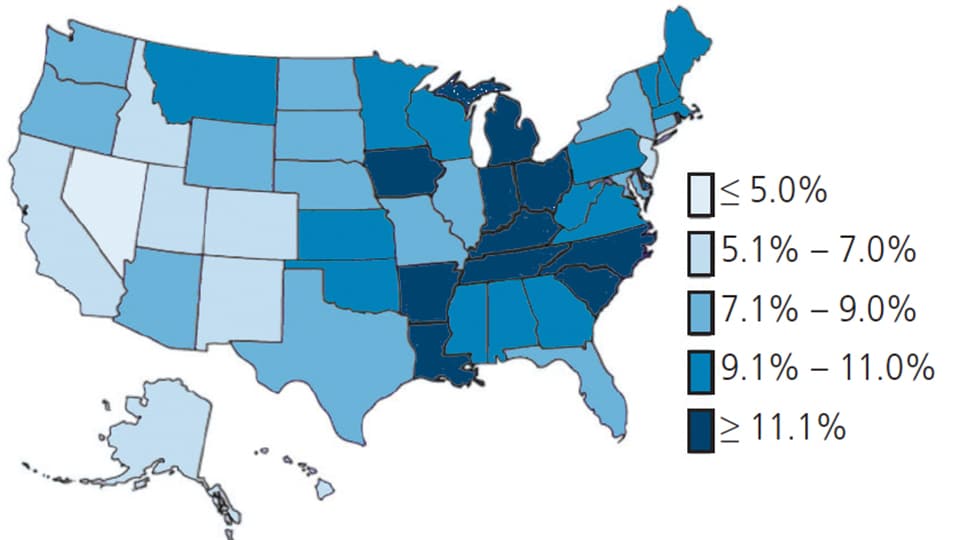
Cross-culturally, there are also significant differences in prevalence — for example, rates of ADHD diagnoses are highest among non-Hispanic white children (11.5%) and lowest among Hispanic youth (6.3%).11 Research has indicated that minority youths (e.g., Hispanics) are less likely to have a parent-reported diagnosis.12 This could possibly be related to a genetic advantage or a decision not to seek medical care for the symptoms (which could be related to cost factors, perceived stigma or not viewing ADHD as a true disorder). Although rates among Hispanics remain lower than non-Hispanics, increasing rates in recent years among Hispanics may indicate a shift in the cultural acceptance of ADHD and/or changes in access to health care.9
COMORBIDITIES AND COST
There is increasing awareness in the comorbidities associated with ADHD. Externalizing disorders are highly prevalent among affected individuals; in fact, approximately 50% to 60% of individuals with ADHD also meet diagnostic criteria for oppositional defiant disorder.13 Compared to their peers without ADHD, affected adolescents are at higher risk for delinquency and substance use.14,15 In addition to externalizing disorders, youth with ADHD are at risk for internalizing disorders. Approximately 25% of these children experience anxiety that may include separation anxiety, generalized anxiety, phobias or obsessive/compulsive disorders.16 These individuals are also at increased risk for developing mood disorders.17 Research indicates that 44% of individuals with a history of ADHD will experience depression, compared to 25% of individuals without ADHD.18 Furthermore, adolescents with ADHD are more likely to attempt suicide than those without such history (12% vs. 1.6%).19 A bipolar condition is also prevalent in youth with ADHD — with rates reported as high as 11% to 22%, compared to 0.3% in the general population.20
The economic costs of ADHD are high. Between $143 billion and $266 billion (adjusted to 2010 U.S. dollars) are spent every year in this country. Most of these costs are incurred by adults due to loss of productivity and income; the main costs for children are seen in health care and education.21
TREATMENT
Treatment can relieve many of the disorder’s symptoms and impairment. Current treatments focus on reducing symptoms and improving functionality in school, work, at home and with peers.9 Behavioral interventions, stimulant medication or a combination of the two are the established therapies for reducing ADHD-associated impairment.
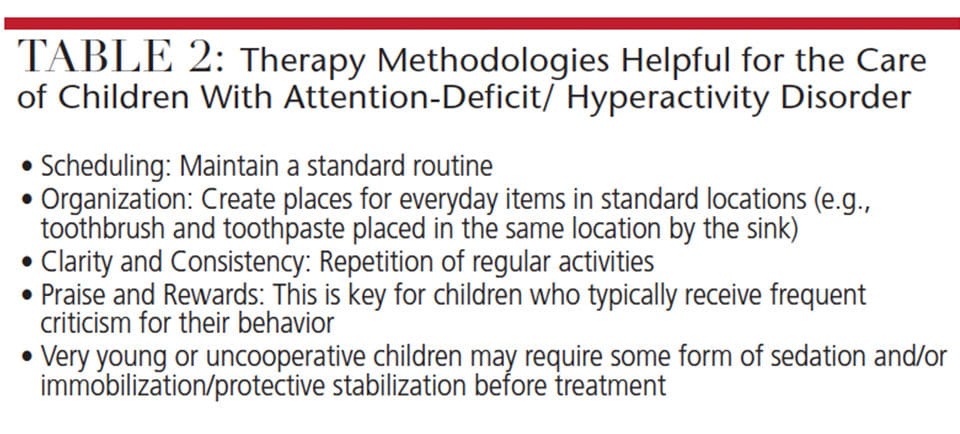
Behavioral treatment typically consists of training parents/caregivers and teachers to reinforce positive behavior while decreasing negative behavior. These programs help parents/caregivers and teachers understand ADHD and oppositional behavior, and help the child increase his or her attention to positive behaviors. Examples include establishing consequences for positive and negative behavior at home — say, by setting up a token economy in which children earn privileges or rewards for meeting goals, or equating good behavior at school to privileges, rewards and fun activities, such as computer time or recess. These interventions can also help youth learn organizational and planning strategies (Table 2).9
Stimulant medication is another evidence-based treatment for ADHD. Research demonstrates these medications are extremely effective in reducing behavioral problems in the short-term, and offer some symptom-management benefit in the long term. Stimulants have produced behavioral improvements in terms of attention and impulse control.9
ORAL HEALTH
Studies also show that patients with ADHD are at increased risk of caries, periodontal disease and bruxism associated with poor oral hygiene, increased consumption of sugary foods, and medication use. As such, it is imperative that this patient population receive regular oral health care.22–28
A full range of dental procedures can be provided to adults and children with ADHD. For children, positive reinforcement for desired behaviors and completed tasks — in addition to consequences for incomplete work — will gradually shape a child’s behavior. In order to increase the likelihood of a successful dental appointment, children with ADHD should be given frequent breaks and offered positive reinforcement for appropriate behavior. They can also be given the opportunity to earn rewards throughout the visit that can be traded for a larger reward at the end. Verbal praise is an important component in reinforcing good behavior; for example, providers (and other adults) should recognize and compliment the children’s positive behavior.
Children with ADHD who are taking stimulant medications may be more cooperative during visits earlier in the day. Extended-release medication typically lasts between 8 and 12 hours and may not be effective during after-school hours.29 One of the symptoms of ADHD is difficulty following directions.3 Behavioral interventions focus on teaching parents/caregivers to provide clear and concise commands. Therefore, the use of repeated, simple instructions can improve self-care compliance. Instructions can also be presented in a creative (e.g., colorful and highly stimulating) manner to keep the child’s attention. Clinicians should use similar methodologies during visits.
It is also important for dental professionals to involve parents/caregivers in the child’s care by focusing on the frequency of oral hygiene routines. Parents/caregivers can provide explicit instructions and subsequent rewards for the successful completion of daily brushing. These techniques will potentially result in increased self-care compliance.30 Oral health providers should take the time to thoroughly review the patient’s medical history and associated conditions, and watch for possible signs and symptoms of physical abuse. Though orofacial injuries may be more common in children with ADHD (in part, due to running or climbing in inappropriate and dangerous situations), these individuals are five to seven times more likely than their non-ADHD peers to experience physical abuse by parents/caregivers.31
While hyperactive symptoms tend to manifest as “inner restlessness” in adolescence and adulthood,32 behavioral difficulties may be less noticeable in adults with ADHD. Nonetheless, dental professionals can utilize strategies to ensure these patients have successful dental appointments. Adults with ADHD can have difficulty remembering appointments, especially if they are outside of their normal routine. In the case of appointments occuring every six months, it may be helpful for dental teams to provide more reminders than usual. For example, in addition to providing a reminder 24 hours prior to the appointment, the staff may also wish to remind patients the morning of their appointment.33
It also may be helpful for appointments to be scheduled in the morning when individuals with ADHD aren’t fatigued and less likely to forget about their appointment later in the day. As with all patients, a comprehensive medical history should be taken at each visit, including a full list of medications (especially those causing xerostomia) and any illicit substance use. This patient population may not be able to comply fully with self-care regimens because of inattention.33 In addition, symptoms in adults are associated with smoking and caffeine consumption, suggesting that adults with ADHD may be self-medicating with caffeine and nicotine to improve their cognitive abilities.34
For children and adults with ADHD, a preventive program — such as caries management by risk assessment — should be followed, with an emphasis on improving salivary quality, remineralization strategies, decreasing risk factors, and increased the frequency of preventive appointments.30
Ultimately, when faced with patients who are inattentive, restless and noncompliant with self-care routines, ADHD should be considered as a causative factor in these behaviors. These patients require compassion, understanding and creativity in determining effective oral health care measures.
REFERENCES
- U.S. Centers for Disease Control and Prevention. Attention-Deficit/Hyperactivity Disorder (ADHD). Available at: cdc.gov/ncbddd/adhd/. Accessed April 12, 2017.
- Hechtman L, Swanson JM, Sibley MH, et al. Functional adult outcomes 16 years after childhood diagnosis of attention-deficit/hyperactivity disorder: MTA results. J Am Acad Child Adolesc Psychiatry. 2016;55:945–952.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Arlington, VA: American Psychiatric Publishing; 2013.
- Pelham WE Jr, Fabiano GA, Massetti GM. Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:449–476.
- Pearcy MT, Copton JR, Pope AW. Influences on teacher referral of children to mental health services: Gender, severity, and internalizing vs. externalizing problems. J Emot Behav Disord. 1993;1:165–169.
- Thurston IB, Phares V, Coates EE, Bogart LM. Child problem recognition and help-seeking intentions among black and white parents. J Clin Child Adolesc Psychol. 2015;44:604–615.
- Biederman J, Faraone SV, Mick E, et al. High risk for attention deficit hyperactivity disorder among children of parents with childhood onset of the disorder: a pilot study. Am J Psychiatry. 1995;152:431–435.
- Levy F, Hay DA. Attention, Genes and ADHD. Philadelphia: Psychology Press; 2001.
- Smith BH, Barkley RA, Shapiro CJ. Attention-deficit/hyperactivity disorder. In: Mash EJ, Barkley RA, eds. Treatment of Childhood Disorders. 3rd ed. New York: Guilford Press; 2006:65–136.
- Visser SN, Bitsko RH, Danielson ML, et al. Treatment of attention deficit/hyperactivity disorder among children with special health care needs. J Pediatr. 2015;166:1423–1430.
- Pastor PN, Reuben CA. Racial and ethnic differences in ADHD and LD in young school-age children: Parental reports in the National Health Interview Survey. Public Health Rep. 2005;120:383–392.
- Pastor PN, Reuben CA, Duran CR, Hawkins LD. Association between diagnosed ADHD and selected characteristics among children aged 4–17 years: United States, 2011–2013. Hyattsville, MD: National Center for Health Statistics; 2015. NCHS data brief, No 201.
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice and DSM-V. J Am Acad Child Adolesc Psychiatry. 1997;36:1065–1079.
- Molina BS, Pelham WE Jr. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. J Abnorm Psychol. 2003;112:497–507.
- Sibley MH, Pelham WE, Molina BS, et al. The delinquency outcomes of boys with ADHD with and without comorbidity. J Abnorm Child Psychol. 2011;39:21–32.
- Jarrett MA, Ollendick TH. A conceptual review of the comorbidity of attention-deficit/hyperactivity disorder and anxiety: Implications for future research and practice. Clin Psychol Rev. 2008;28:1266–1280.
- Meinzer MC, Pettit JW, Viswesvaran C. The co-occurrence of attention-deficit/hyperactivity disorder and unipolar depression in children and adolescents: A meta-analytic review. Clin Psychol Rev. 2014;34:595–607.
- Meinzer MC, Lewinsohn PM, Pettit JW, et al. Attention deficit-hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depress Anxiety. 2013;30:546–553.
- Chronis-Tuscano A, Molina BS, Pelham WE, et al. Very early predictor of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2010;67:1044–1051.
- Klassen LJ, Katzman MA, Chokka P. Adult ADHD and its comorbidities, with a focus on bipolar disorder. J Affect Disord. 2010;124:1–8.
- National Resource Center on ADHD. Cost of ADHD. Available at: chadd.org/understanding-ADHD/About-ADHD/Data-and-Statistics/Cost-of-ADHD.aspx. Accessed April 12, 2017.
- Chandra P, Anandakrishna L, Ray P. Caries experience and oral hygiene status of children suffering from attention deficit hyperactive disorder. J Clin Pediatr Dent. 2009;34:25–29.
- Chau YC, Lai KY, McGrath CP, Yiu CK. Oral health of children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2017;125:49–54.
- Dursun OB, Şengül F, Esin IS, Demirci T, Yücel N, Ömezli MM. Mind conduct disorder in children with poor oral hygiene habits and attention deficit hyperactivity disorder in children with excessive tooth decay. Arch Med Sci. 2016;12:1279–1285.
- Blomqvist M, Holmberg K, Fernell E, Ek U, Dahllöf G. Dental caries and oral health behavior of children with attention deficit hyperactivity disorder. Eur J Oral Sci. 2007;115:186–191.
- Bimstein E, Wilson J, Guelmann M, Primosch R. Oral characteristics of children with attention-deficit hyperactivity. Spec Care Dentist. 2008;28:107–110.
- Blomqvist M, Ahadi S, Fernell E, Ek U, Dahllöf G. Dental caries in adolescents with attention deficit hyperactivity disorder: a population-based follow-up study. Euro J Oral Sci. 2011;119:381–385.
- Grooms MT, Keels MA, Roberts MW, McIver FT. Caries experience associated with attention-deficit/hyperactivity disorder. J Clin Pediatr Dent. 2005;30:3–7.
- Charles JM. Dental care in children with developmental disabilities: attention deficit disorder, intellectual disabilities, and autism. J Dent Child (Chic). 2010;77:84–91.
- Francisco EM, Azevedo S, Lyon LJ, Horlak DJ, Watson PD, Young DA. Managing the risk of caries. Dimensions of Dental Hygiene. 2008;6(10):44–45.
- Waldman HB, Swerdloff M, Perlman SP. You may be treating children with mental retardation and attention deficit hyperactive disorder in your dental office. J Dent Child. 2000;67:241–245.
- Kooij SJ, Bejerot S, Blackwell A, et al. European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD. BMC Psychiatry. 2010;10:1–24.
- Friedlander AH, Yagiela JA, Mahler ME, Rubin R. The pathophysiology, medical management and dental implications of adult attention-deficit/hyperactivity disorder. J Am Dent Assoc. 2007;138:475–482.
- Dosh T, Helmbrecht T, Anestis J, Guenthner G, Kelly TH, Martin CA. A comparison of the associations of caffeine and cigarette use with depressive and ADHD symptoms in a sample of young adult smokers. J Addict Med. 2010;4:52–54.
FEATURED IMAGE BY LINDA EPSTEIN/ISTOCK UNRELEASED/GETTY IMAGES PLUS
From Decisions in Dentistry. May 2017;3(5):52—55.